Urinary Infection (Urinary tract infection)
What is Urinary Tract Infection?
Urinary tract infection is the name given to various inflammatory conditions that occur in the urinary tract. It occurs more frequently in the lower urinary tract. In lower urinary tract infections, the inflammatory condition occurs in the urinary tract called the bladder and urethra where urine is transported out of the kidneys. Urinary tract inflammation in the bladder is called cystitis. Cystitis is the most common form of infection in the lower urinary tract. Lower urinary tract infections are usually harmless.
It consists of the upper urinary tract, the kidneys and the duct called the ureter that connects the kidneys to the bladder. Infections that occur in this part are more dangerous. It is most commonly seen in the renal pelvis, the junction of the ureters with the kidneys, and inflammation of this region is called pyelitis.
What Causes Urinary Tract Infection?
The underlying cause of urinary tract inflammation is an infection caused by bacteria in most cases. These are often ascended from the urethra and are mainly intestinal bacteria of the Escherichia coli species, originating from one’s faeces. Rarely, a sexually transmitted pathogen such as gonococcus and chlamydia, virus or fungus may also be the causative agent.
What are the Symptoms of Urinary Tract İnfection?
Urinary tract infection symptoms typically manifest as burning or frequent urination during urination. But it can be seen without any symptoms. Common symptoms of urinary tract infection are;
- Burning or pain in urine,
- Frequent need to urinate,
- The weakening of urine flow,
- Difficulty keeping urine,
- Blood in urine,
- Pain in the lower abdomen.
In upper urinary tract infections with renal involvement;
- Kidney sensitivity,
- Side pain,
- Fire,
- Nausea/vomiting,
- Symptoms such as general weakness may also occur.
How Does Urinary Tract Infection Treat?
Uncomplicated inflammation of the lower urinary tract is easy to treat and heals quickly with timely intervention. Although 30 to 50% of uncomplicated urinary tract infections heal spontaneously and without damage, oral antibiotic therapy is recommended to reduce the inconvenient clinical symptoms more quickly and to eliminate pathogens. Also, infections with the urinary tract, renal involvement may cause permanent damage if not treated early.
- If there is a pain or burning sensation while urinating, if the only incision can be made, contains blood, or if severe abdominal pain is added later, a visit to a doctor is recommended.
- Uncomplicated treatment of urinary tract infection is usually done with antibiotics.
- After taking antibiotics, inflammation begins to regress within a few days.
- In addition to antibiotics, painkillers or antispasmodic drugs may be used.
- Recurrent urinary tract infections require high doses of antibiotic therapy.
- Pregnancy, diabetes, immunosuppressed people and children are planned by the treatment conditions.
Painful Bladder Syndrome (Interstitial Cystitis)
What is Painful Bladder Syndrome (Interstitial Cystitis)?
It is a type of chronic cystitis. In this type of bladder wall significantly thickens and limits the working capacity of the bladder. Although the cause is not known, it can be explained that the covering the urinary bladder and preventing the passage of urine to the inner layers is damaged for various reasons and the urine populates the inner layers causing inflammation.
What are the Symptoms of Painful Bladder Syndrome (Interstitial) Cystitis?
- Continuous urination and low status
- Pain during sexual intercourse
- Pain and burning sensation in the vagina, inside the urinary tract, between the so-called “roof” and the pelvis, even when there is no urination
- Pain that can begin 2-24 hours after sexual intercourse
How to Diagnose?
- Urine diary,
- Urine analysis and culture,
- Gynaecological examination (this is a very useful method for the urologist experienced in making the diagnosis),
- Imaging of the inner surface of the bladder by Endoscopy (Cystoscopy) under general or regional anaesthesia.
Endoscopy (Cystoscopy)
This is one of the most important methods in diagnosis. Under general or regional anaesthesia (numb below the waist), we can see the inside of the bladder with the camera and, most importantly, reveal the actual volume (capacity) of the bladder under anaesthesia. If the capacity is lower than required (1000-1200 ml), the diagnosis is made. One of the most important advantages of performing endoscopy is to increase the decreased capacity by inflating the bladder under anaesthesia.
How is it Treated?
For Painful Bladder Syndrome, many available treatment options are used to help alleviate symptoms, such as bladder pain, sudden and frequent urination. The patient can also support his treatment with the diet he will apply to reduce disease attacks.
Hyperactive Bladder (Overactive bladder)
What is an Overactive Bladder?
Overactive bladder; urinary bladder (bladder) muscle is a disease that develops as a result of involuntary contractions and social life is highly affected. Under normal conditions, urine in the bladder does not urinate until it reaches a certain volume. However, in the case of overactive bladder, the situation is different. Even a cup of urine can feel very seriously stuck, and even urine can be missed.
What are Overactive Bladder Symptoms?
Urine storage symptoms. Storage symptoms include:
- A sudden need for urination and the inability to postpone it
- Involuntary urinary incontinence
- The need to urinate more often than usual
- Waking up with the need to urinate at night
Causes of Overactive Bladder Symptoms?
Some people experience sudden and spontaneous contractions in their bladder. Some people feel more sensitive to bladder filling. In some cases, the kidneys produce more urine at night. This causes nocturia. This may be related to advanced age and certain medical conditions. Some people have smaller bladders and fill faster. This is not very common.
Terms Available to your Doctor
- Sudden urinary urgency cannot be delayed: the need to urinate causes fear of urinary incontinence.
- Sudden incontinence: incontinence as a result of failure to reach the toilet
- Frequency of urination: Urine sensation at more frequent intervals, usually more than 8 times a day
- Nocturia: Waking up with the need to urinate 1-2 times at night
- LUTS (lower urinary tract symptoms): A term used for all symptoms that affect the urinary tract.
Diagnosis of Overactive Bladder
The doctor may order tests to understand the causes of your symptoms. First of all, the doctor or nurse will take your medical history and carry out your physical examination. If needed, he can do other tests.
Medical background
The doctor will take your detailed medical history and ask questions about your symptoms.
- Tell me how long you have had symptoms
- Make a list of the drugs you take
- Make a list of previous surgical interventions
- Tell us about other diseases
- Describe your lifestyle (such as exercise, smoking, alcohol and diet)
- Physical examination
Your doctor or nurse will examine the following points in your physical examination:
- your stomach
- Your genital area
- your back
- Urine test
You should give him urine for testing. This test can show urinary infection and small amounts of blood or sugar in your urine.
How is Overactive Bladder Disease Treated?
Many patients can be successfully treated with medication. Supporting behavioural therapies along with drug treatment also increases the success rates significantly.
Drug Therapy: Drugs are widely used in the treatment and have proven efficacy and safety. When evaluated in terms of preventing urinary incontinence, their efficacy is between 60% -75%.
Behavioural Therapy: It consists of urine-retaining muscle exercises, compression suppression techniques, changing the time of taking diuretic drugs and directing the patient to lose weight.
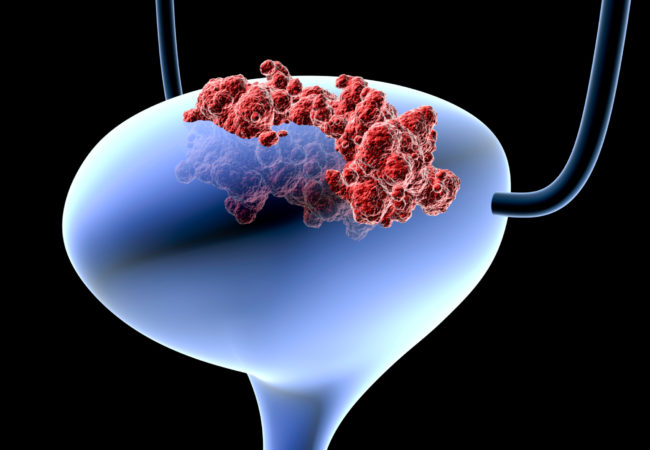
Bladder Cancer
What is Bladder Cancer?
Bladder cancer is caused by abnormal growth of cells within the bladder, also called the bladder, which is responsible for storing urine in the body. The cells in the bladder undergo mutations that cause them to grow and die uncontrollably rather than grow and divide as intended. These abnormal cells can cause tumours in the bladder. These tumours may be benign bladder tumours or malignant bladder tumours containing cancerous cells.
What Causes Bladder Cancer?
Causes of bladder cancer include:
- Smoking and other tobacco products
- Exposure to chemicals, especially in a job requiring exposure to chemicals
- Being exposed to radiation in the past
- Chronic irritation of bladder inner wall
- It is not always clear what causes bladder cancer, and some people with bladder cancer have no apparent risk factors.
What are the Risk Factors in Bladder Cancer?
Nowadays, it is possible to talk about the genetic predisposition of superficial and slowly progressing bladder tumours. Many tumour suppressor genes have been reported to play a role in the formation of bladder cancer.
Against bladder cancer;
- Genetic susceptibility
- Smokers,
- Older people,
- Men
- Excessive consumption of fatty and fried foods,
- Chemical, paint, rubber, leather industry workers,
- Dry cleaner, paper industry, petroleum industry, cosmetic industry, dental technician, gas and aluminium industry workers
- Recurrent urinary tract infection,
- Those with long-term bladder disease,
- Long term catheters or catheters,
- High-dose irradiation to the bladder (increased risk 4-fold),
- Those who receive chemotherapy are at risk.
Bladder Cancer Symptoms
Signs and symptoms of bladder cancer may include:
- Blood in the urine (hematuria)
- Pain in urine
- Pelvic pain
If you have hematuria, your urine may appear bright red or cola coloured. Sometimes urine may not look different, but blood in the urine can be detected by microscopic examination of the urine.
People with bladder cancer may also experience the following symptoms:
- Back pain
- Frequent urination
However, these symptoms are usually caused by a condition other than bladder cancer.
Types of Bladder Cancer
Types of bladder cancer include:
Urothelial carcinoma
Urothelial carcinoma, previously referred to as transitional cell carcinoma, occurs in cells that form the inside of the bladder. When your bladder is full, urothelial cells expand and narrow when your bladder is empty. These cells form the inside of the ureters and urethra, and tumours can also occur in these places. Urothelial carcinoma is the most common type of bladder cancer.
Squamous cell carcinoma
Squamous cell carcinoma is associated with chronic irritation of the bladder, for example, due to an infection or prolonged use of a urinary catheter.
Adenocarcinoma
Adenocarcinoma begins in the cells that make up the mucous secreting glands in the bladder. Adenocarcinoma is also rare.
Some bladder cancers may also include more than one cell type.
How are the Stages of Bladder Cancer Determined?
After confirming that you have bladder cancer, your doctor may recommend additional tests to determine whether your cancer has spread to your lymph nodes or other parts of your body.
Tests may include:
- CT scans
- MRI (Magnetic Resonance Imaging)
- Bone scan
- Chest X-ray
Your doctor uses the information from these procedures to determine the stage of your cancer. The stages of bladder cancer are expressed in Roman numerals from 0 to IV. The lowest stages indicate cancer that is limited to the inner layers of the bladder and is not sufficiently developed to affect the muscle layer of the bladder wall. The highest stage – stage IV – refers to the spread of cancer to lymph nodes or distant organs of the body.
The cancer staging system continues to evolve and is becoming more complex as doctors improve their cancer diagnosis and treatment. Your doctor uses the cancer stage to select the treatments that are right for you.
Bladder Cancer Treatment
Different treatment options are available for bladder cancer, either alone or in combination with each other. Bladder cancer takes many forms and its prognosis changes. Therefore, the correct staging and histopathological classification performed by a pathologist becomes important according to the choice of treatment.
If the tumour is superficial, it is treated by transurethral resection (TURB) of the bladder if it does not spread from the bladder mucosa to the muscle tissue of the bladder. A cystoscope is placed in the urinary bladder and the tumour is scraped or incinerated.
Radical surgery can be selected if cancer has spread to the bladder muscle tissue or is at risk. This means partial or complete removal of the bladder and removal of the prostate. There are two alternatives to urinate after the operation. A urostomy refers to the collection of urine through a stoma into a urostomy bag. Another alternative is to use a portion of the intestine to create a spare bladder.
Continue
Depending on the type of cancer, the size of the tumour and possible metastases, radiotherapy and intravenous chemotherapy may also be necessary. Chemoradiotherapy can be as successful as traditional surgery.
A male patient’s prostate is normally removed during surgery, but the urethra is usually preserved. The urethra of a female patient is removed and usually, the uterus and adnexa are removed. If surgical treatment is not possible, the cancer is treated with radiotherapy for reasons such as the patient’s physical condition or the location of the tumour.
At the time of diagnosis, metastasis occurs in a small minority. In this case, it may be decided not to perform bladder removal and the patient is referred to as radiotherapy or chemotherapy. In metastatic cancers, radiotherapy may be used as a palliative treatment to alleviate the symptoms caused by pain, discharge, a large tumour, or urinary obstruction. Metastatic cancer is treated with chemotherapy.
Cystitis
What is Cystitis?
Cystitis, which means inflammation of the urinary tract, is one of the most common diseases in the urinary tract and reproductive system. Cystitis, whose incidence is much higher in women, is caught by at least 20 per cent of women at least once in their lifetime.
What are the Symptoms of Cystitis?
- Burning and draining while urinating (may persist after urinating),
- Frequent urination,
- The spread of pain to the groin and the breech,
- Fire,
- Sweating,
- Fatigue,
- Vomiting and nausea,
- Your urine may be cloudy, smelly.
- There may be pain during sexual intercourse.
How is Cystitis Diagnosed?
A urologist can diagnose based on the description of the complaints and the tests. These tests include urine analysis, cystoscopy, and a special X-ray called intravenous pyelogram. These examinations are performed to investigate the factors that predispose to infection. A urine culture may also be required to identify the bacterium that causes the infection. Cystitis is not an important disease if treated promptly and appropriately. If cystitis and its underlying cause are not treated, it will become chronic and debilitating.
What Causes Cystitis?
Normally bacteria; they live in the reproductive organs and anus. Sometimes these bacteria cross the lower urinary tract and reach the bladder. Bacteria that reach the bladder are expelled by urination. However, if the number of bacteria coming to the bladder is more than the discarded, they cause inflammation in the bladder and later in the kidneys.
Transmission can occur during sexual intercourse or when genital cleansing is low, as well as prolonged urinary retention, urinary tract contraction diseases, and low estrogen levels in menopause.
Since the urethra is much shorter in women than in men, it is easier for bacteria to reach the bladder from the outside. Therefore, the incidence of cystitis in women is much higher. At least 20 per cent of women has cystitis once in their lifetime.
The most common cause of cystitis is Escherichia coli (E.coli, coli bacillus) microorganism. This bacteria can be found normally in the large intestine and can reach the bladder through sexual intercourse.
What is Cystitis Treatment?
Cystitis is treated with antibiotics. Before starting treatment, samples should be taken for urine culture and antibiogram, effective antibiotics should be used in urinary tract infections until results are obtained, and if necessary, these drugs should be changed according to antibiogram results. Treatment may be prolonged in chronic infections.
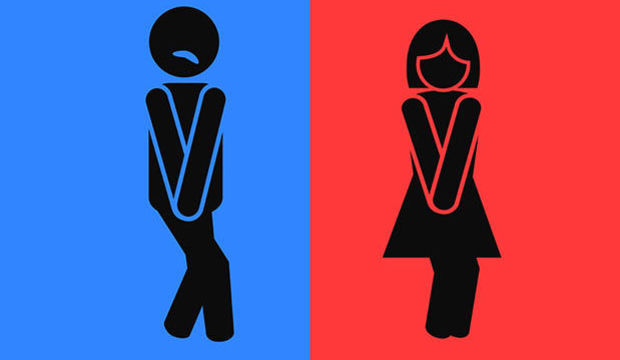
Urinary Incontinence
What is Urinary Incontinence?
Urinary incontinence is uncontrolled and unwanted incontinence. If this condition recurs regularly, it is considered a medical problem. Women complain more about urinary incontinence than men.
Many patients remain untreated because they feel uncomfortable talking to their doctor about urinary incontinence.
Causes of Urinary Incontinence
The most common causes of urinary incontinence:
- Hormone deficiency
- The weakness of pelvic floor muscles
- Urinary incontinence due to neurological diseases
- Urinary tract infection
- Prostate enlargement
Common risk factors:
- Previous pelvic surgery
- Previous prostate surgeries
- Birth
- Menopause
Urinary incontinence becomes more common with increased age. But ageing is not a normal process.
How Many Types Of Urinary Incontinence
There are 3 types of incontinence problems.
Dependent on pressure: Urinary incontinence while coughing, sneezing, exercising, doing sports
Type of impingement: Urinary incontinence due to a sudden contraction of the bladder
Overflow type: If the patient does not notice that the urine comes in due to decreased sensitivity of the bladder or nerve injuries, and consequently incontinence
How is Urinary Incontinence Diagnosed?
Firstly, a detailed history is taken from the patient. The conditions that initiate urinary incontinence and the type and frequency of incontinence are learned. Patient; blood sugar, urinalysis and urine culture, ultrasound and urodynamics may be requested. If the underlying cause is considered, the related investigations are performed.
How Is Urinary Incontinence Treated?
If the patient has excess weight, it is ensured that it is weakened by an appropriate diet and exercise program. If the reason is constipation, the diet is regulated and medication is given. If the cause of uncontrolled diabetes, the patient’s medications and diet are regulated. Excessive fluid intake is prevented. Patients who smoke and drink excessively are asked to reduce them. Urinary tract infections are treated with appropriate antibiotics. Strengthening exercises of the bladder and pelvic muscles is recommended. These exercises are based on the principle of retention and release of urine while urinating.
There are also medications used in cases of incontinence. These are given by urologists to appropriate patients. If urinary incontinence is caused by prostate enlargement, bladder sagging, surgery may be considered.
If you have problems with urinary incontinence, it is very important to see a urologist. If the problem is left untreated, it may cause skin rash and infections. Urinary incontinence can also be a precursor to some diseases. Also, incontinence reduces a person’s self-esteem, creates a sense of shame. Therefore, even patients may apply to the doctor late. Your physician will ask for a detailed history and physical examination after a physical examination; will apply the treatment method that will be useful to you.
Kidney Failure
What is Kidney Failure?
Renal failure of the kidneys due to various diseases is called partial or total failure.
Types of Kidney Failure
The causes of renal failure are divided into 5 main categories:
1) Acute Prerenal Renal Failure: Acute prerenal renal failure occurs when blood flow to the kidneys decreases. Because the blood flow is insufficient, the kidneys cannot fully filter the blood. This type of renal insufficiency can usually be treated by correcting the condition that affects blood flow.
2) Acute Internal Renal Failure: Acute internal renal failure occurs as a result of traumas directly affecting the kidneys. Accidents, blows to the kidneys, toxin loading, not enough oxygen to the kidneys, excessive blood loss, renal infections are among the causes of internal renal failure.
3) Chronic Prerenal Renal Failure: When acute prerenal renal failure is not treated and the kidneys are unable to clear the blood, the condition becomes an acute internal renal failure. In this case, the kidneys begin to shrink and gradually lose function.
4) Chronic Internal Renal Failure: Strokes, traumas and untreated kidney infections in the kidneys cause acute internal renal failure to turn into chronic internal renal failure.
5) Chronic Postrenal Renal Failure: This type of renal failure occurs as a result of the obstruction of the urinary tract for a long time and the urine cannot be excreted completely from the body.
Causes of Acute Renal Failure
- Pregnancy poisoning
- Unhealthy abortions
- Heart failure
- Kidney Diseases
- Obstruction of urinary tract
- Some long-term medications
- Major and serious surgeries
- Decreased blood flow
Causes of Chronic Renal Failure
- Diabetes
- Hypertension
- Kidney cyst
- Renal inflammation
- Vesicoureteral reflux
How is Kidney Failure Diagnosed?
Your doctor will perform a physical examination after you have learned what are the symptoms that attract your attention. It may ask how much urine you have during the day and if you have any problems when you urinate.
Various tests and procedures are used to make a complete diagnosis of renal failure. Urine and blood tests will help your doctor determine if the kidneys are functioning properly.
Imaging methods such as ultrasound and/or CT scan may be used to see if there is any change in the size of the kidneys.
In some cases, a kidney biopsy may be required.
Treatment of Renal Failure
Treatment of renal failure, which is divided into acute and chronic, is also different. First of all, the treatment that should be under the control and supervision of the doctor varies according to the factors causing the disease. Another important factor to be considered in the treatment is the control of blood pressure is low. In addition to this, apart from drug therapy, treatment with nutrition should be supported. Early diagnosis is very important in the treatment of renal failure. Otherwise, treatments such as dialysis and kidney transplantation can be applied in progressive and permanent renal failure.
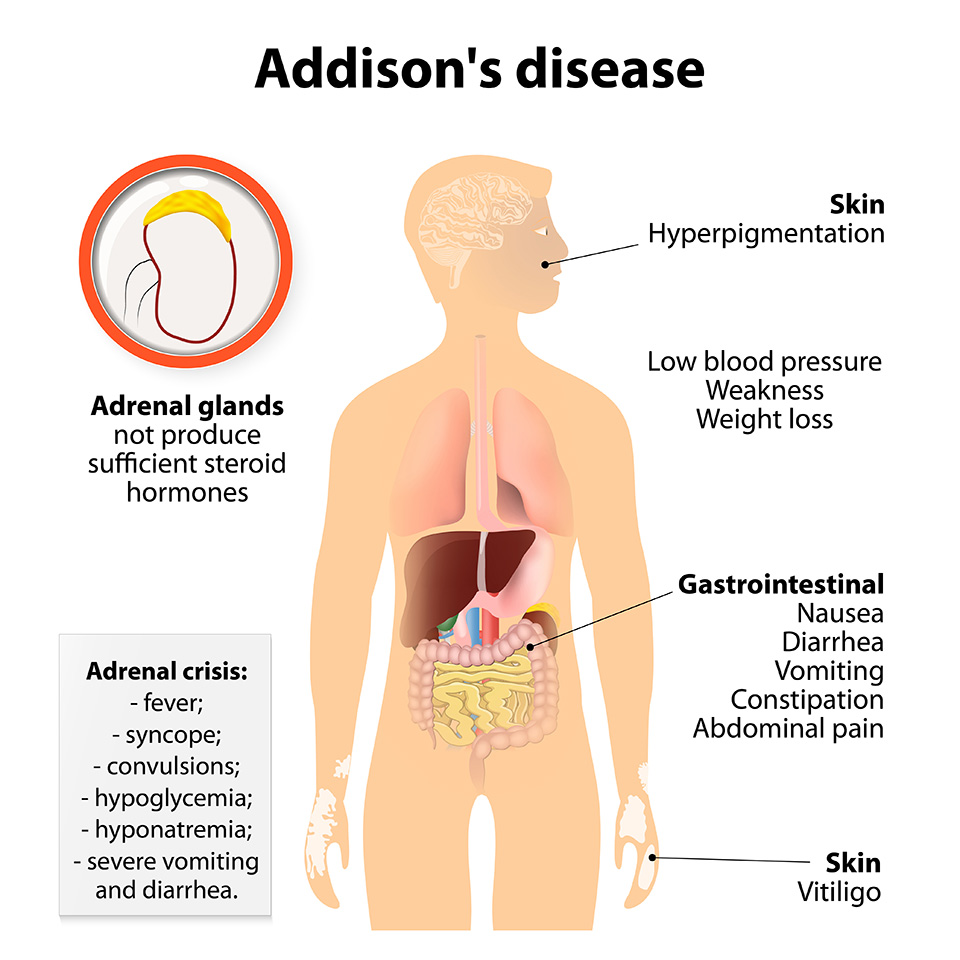
Addison’s Disease (Hypoadrenocorticism)
What is Addison’s Disease?
Addison’s disease is caused by the damage of the adrenal crust and the inability of the adrenal glands to produce enough cortisol and aldosterone hormones.
Why Addison Disease?
There are two types of Addison’s disease:
Primary adrenal gland failure and secondary adrenal gland failure. Approximately 70% of primary adrenal insufficiency is due to an autoimmune process. Other causes such as adrenal gland damage, tuberculosis, various bacterial, virus and fungal infections, adrenal haemorrhage and metastasis of cancer to the adrenal glands may also cause primary adrenal insufficiency.
Secondary adrenal gland insufficiency occurs due to the decrease in pituitary hormone ACTH (adrenocorticotropic hormone) production. Cortisol production is not stimulated in the absence of ACTH due to a pituitary tumour or other cause. Aldosterone production is generally unaffected in secondary adrenal insufficiency.
What are the Symptoms of Adrenal Failure?
Many symptoms are seen in people with adrenal insufficiency (Addison’s disease). In general, the symptoms are as follows:
- Chronic fatigue and muscle weakness
- Increased skin pigmentation (skin becomes darker)
- Weight loss decreased appetite and difficulty digestion
- The decrease in heart rate and blood pressure
- Low Blood Sugar
- Fainting
- Pain in the mouth
- Salt request
- Nausea
- Vomiting
- Nervousness and depression
- Stress relief
- Increased sensitivity to hot and cold
How to Diagnose Adrenal Failure?
People with adrenal insufficiency may not understand the symptoms of the disease. Therefore, discomfort may progress. The distinctive symptoms of adrenal insufficiency are:
- Sudden severe pain in the waist, abdomen or legs
- Excessive fluid loss following severe vomiting and diarrhoea
- Rapidly falling blood pressure
- Loss of consciousness
- Kidneys become unable to do their job
People with these signs and symptoms should seek medical advice immediately. After asking for signs and symptoms, the physician performs a physical test. Measures of potassium and sodium levels. It also determines hormone levels.
How is Addison’s Disease Treated?
Because adrenal insufficiency causes the absence of functional hormones for the body, doctors often apply hormone replacement for Addison’s disease treatment. This is done once or twice daily with hydrocortisone tablets, which is a steroid hormone. If necessary, aldosterone can be replaced with a synthetic steroid, fludrocortisone acetate, taken orally once a day. These medications should be increased especially during times of stress, infection, surgery or injury. Hormone treatment is usually successful. Once treatment is successful, people with Addison’s disease can lead a fairly normal life. However, it is recommended that they always carry a doctor’s alert bracelet and emergency ID card and keep a small source of medication at work or school.
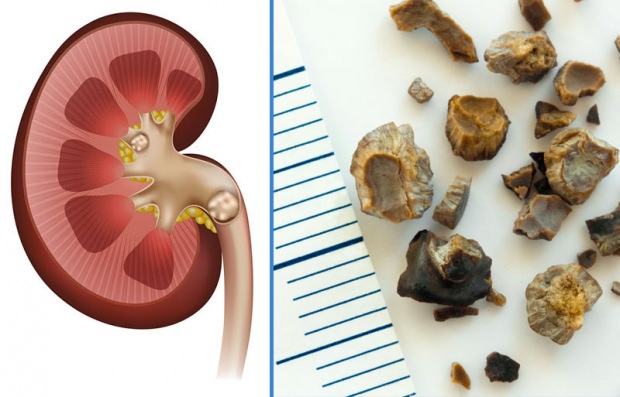
Kidney Stone
What is Kidney Stone?
Kidney stones are hard masses with mineral content formed within the renal canals.
The reason and mechanism of the formation of the stones are unknown.
Stones are common in people with congenital urinary tract abnormalities, family history of kidney stones, and suffering from a systemic disease (gout, etc.).
What is the İncidence of Kidney Stones?
Kidney stones are seen more frequently in men, 3 times more than women.
What are the Conditions that İncrease Kidney Stone Formation?
Frequent urinary tract infections, kidney diseases such as cystinuria and systemic diseases such as gout increase the formation of kidney stones. Kidney stone formation is also common in chronic intestinal inflammation.
Other than diseases; not taking enough fluid during the day, stone history in the family, being in the age range of 30-50 years, sedentary lifestyle are factors that increase stone formation.
What are the Symptoms of Kidney Stones?
- Severe flank – side pain
- Nausea
- Vomiting
- The presence of blood in the urine (which may be microscopic) is a common symptom.
How is Kidney Stone Diagnosed?
Imaging methods and laboratory tests are used in the diagnosis of kidney stones.
Direct X-ray or ultrasonography is used to detect the stone.
In the absence of visualization, computed tomography is requested and this method gives the definitive diagnosis.
How is Kidney Stone Treatment Done?
Kidney stones up to 5 mm are treated with painkillers, antispasmodic drugs and plenty of fluids due to the small size of the stone. With these methods, the stone may fall spontaneously.
Kidney stones larger than 5 mm are treated with ESWL (breaking stone with shock waves from outside the body) and excreted in the urine.
PNL (Percutaneous Nephrolithotomy): An endoscopic (closed) operation, the PNL method is used for the treatment of kidney stones that are larger than 2 cm and cannot be broken by ESWL. The patient underwent a 1 cm incision from the waist area under general anaesthesia. By entering through this incision, the stones are removed as a whole or broken. In this method, the breakage of stones is broken by pneumatic, ultrasonic or laser stone breakers.
URS (Ureteroscope): If stones in the ureter cannot fall or break with ESWL, they are broken and treated with a ureteroscope. Ureteroscopes are devices with a diameter of 2.5-3 mm and a lens that provides an image. Patients are discharged home on the same day after treatment.
Urinary Tract Stenosis
Urinary tract stenosis, which may occur due to infection or impact, is a very victimizing situation. The disease, which presents with symptoms such as difficulty in urination or pain, can be easily treated with different methods.
What is Urinary Tract Stenosis?
If the urinary bladder and the urethra, the last part of the urinary canal, are damaged for any reason, scar tissue may be created which reduces the width of the canal and may slow down or in some cases completely inhibit the flow of urine and/or semen.
The urethral strictures in the urethra,
- The slowdown in urine flow
- Pain when urinating
- Bifurcation and scattering of urine
- After urinating, it may show by dripping.
Causes of Urinary Tract Stenosis
The most common cause of these strictures in the urinary tract is previous infections. Also, interventions such as catheter insertion from the urinary canal and surges from outside can cause scarring in the urinary canal and thus cause stenosis.
How Is Urinary Tract Stenosis Diagnosed?
Uroflowmetry, which is a computerized measurement of urine flow rate, is the first diagnostic test for patients with suspected stenosis. According to the results obtained in this examination, the patient may be directed to retrograde urethrography imaging. In this imaging method, the structure of the urinary tract is revealed by fluoroscopy by filling the urinary canal with the contrast agent which gives an opaque image under x-rays.
Types of Treatment
1) Urethrotomy intern
Urethrotomy intern, known as “closed surgery arasında among the people, involves entering the urine hole through the special devices with a camera and light source at the end and proceeding to the point of stenosis and cutting the stenosis with a cold knife under direct vision. Because it is a painless and quite simple procedure for the postoperative patient, it is usually the first choice in non-advanced urinary tract strictures.
This procedure, which is performed under general or spinal anaesthesia, takes between 20 minutes and 1 hour depending on the type of stricture. The patient is implanted with a urinary catheter during surgery and is usually discharged on the same day.
Antibiotics and painkillers will be given for post-operative use. Urine catheter is taken approximately 3 days later. To prevent recurrence of the stenosis, the urinary catheter was tried to be held for a period of up to 6 weeks, but it has been shown in scientific publications that the long duration of the catheter does not make a significant difference compared to the 3 days. Although you may return to work and life on the following day, it is advisable to stay away from heavy sports and sexual intercourse for two weeks after the operation.
Considering the simplicity of the procedure, urethrotomy intern is recommended as the first treatment option for all patients with stenosis shorter than 1 cm. If the patient repeats stenosis, the second urethrotomy is recommended to other treatment options since it is not possible to increase success with the intern procedure.
2) Urethra dilatation
Urethral dilatation, which is based on regular dilation of the urinary canal performed by the doctor or the patient with a hard catheter or spark plug, was widely used to prevent recurrence of strictures after urethrotomy. Recent studies have shown that even if applied twice a week and for 1 year, it cannot prevent the recurrence of the stricture and can only extend the period until the development of the stricture.
Urethral dilatation is performed under the conditions of a polyclinic or at home with the help of special gels containing a local anaesthetic. The patient may return to daily activity immediately after dilatation and does not need to use any medication.
3) Urethral stents
Urethral stents are similar to cardiac stents in both appearance and function. The aim is to create an expandable lattice structure that is placed inside the urinary stenosis. This process is usually effective in shorter strokes with less depth. It should be noted that these structures are also the most easily treatable strictures by internal urethrotomy and open surgery.
Although stenting is usually performed under regional anaesthesia, it can also be applied under local anaesthesia supported by sedation. The procedure lasts approximately 30 minutes and the patient usually does not receive a urinary catheter after the procedure. The patient is rested for several hours after the operation and discharged.
4) Open surgery
Open surgery has a high success rate of 85% that no other treatment can offer. In open surgery, the aim is to remove the narrowing portion of the urinary tract and to reattach the intact ends. During this treatment, if the urinary canal stenosis is too long, the intact ends may be too far apart to be joined together. In such a case, a patch is taken from another point of the body to close the remaining space. The most commonly used material for this is the “mucosa”, the skin that covers the mouth, while different patch materials such as skin, tunica albuginea, tensor fascia lata can also be used.
Open surgery can be performed under general anaesthesia or spinal anaesthesia. The operation takes between 1 and 2.5 hours depending on the location and length of the stenosis. You are usually asked to stay in the hospital one night after surgery. Pain and antibiotics will be given during discharge. The urinary catheter inserted during the operation will be taken after 10 to 21 days depending on the repair of the stricture. After approximately 4 days you will be able to follow your daily routine with your catheter.
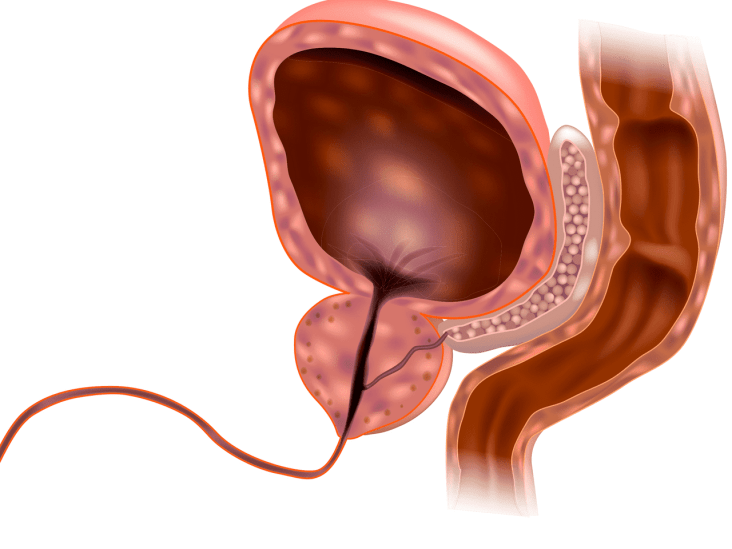
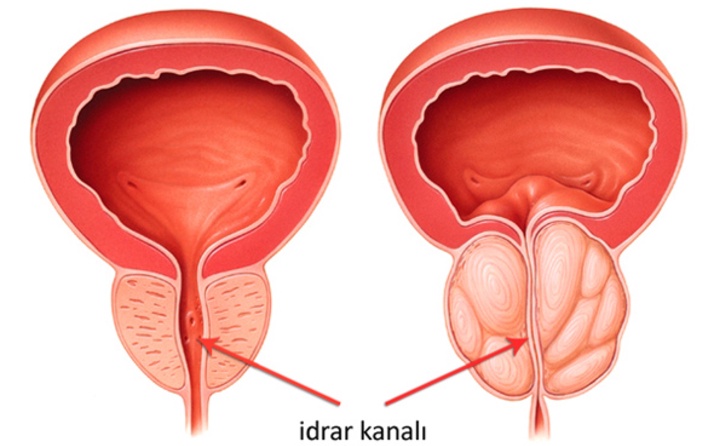
Prostate Diseases
The prostate is a secretory organ found in males, approximately the size of a walnut, located under the bladder, producing various secretions for reproductive activities. Prostate Enlargement, also known as Benign Prostatic Hyperplasia (BPH), is a disease commonly known as benign prostate enlargement.
Studies have shown that benign prostate enlargement is seen in 25% of men aged 50 and 90% of men aged 80 years.
Reasons
Although the exact cause of prostate enlargement is unknown, ageing is the best-known cause. Genetic factors are effective in prostate enlargement, and it is more common in patients with a family history of prostate enlargement.
Also, although some environmental factors and their relationship with nutrition have been studied, no satisfactory net results have been obtained.
In recent years, studies have been conducted to show the relationship between obesity and prostate enlargement. Accordingly, increased body weight, body mass index, and around the umbilicus are associated with an increase in prostate size.
Symptoms
As the prostate grows, it starts to block the urine flow by blocking the urinary tract. Depending on the degree of obstruction, patients have some complaints about urination.
Symptoms of prostate enlargement include:
- Reduction of urine flow intensity,
- Difficulty in starting urine,
- Interruption of urination,
- The feeling of not fully emptying the urine,
- Frequent urination,
- Sudden impingement attacks,
- Urinary incontinence,
- Bifurcation of urine and urination at night.
Diagnostic Methods
Patients with the above complaints should be examined for Benign Prostatic Hyperplasia – BPH. PSA (Prostate-specific antigen) assay, urine analysis and rectal examination and additional examination methods, if necessary, should be demonstrated to be benign in prostate growth.
If there is no abnormality, the patient is considered to have prostate enlargement. Ultrasonography (USG) and Uroflowmetry are performed to determine the degree of prostate enlargement.
Treatment Methods
In the case of prostate enlargement, the bladder cannot be emptied and the remaining urine can cause recurrent infections and permanent impairment of renal function.
At the same time, the complaints of prostate enlargement, the quality of life of the patients are very low. “Prostate enlargement is a disease that needs treatment.”
In prostate enlargement (BPH), patients who do not respond to drug treatment and who initially respond to drug treatment become insufficient over time and cannot use the drug due to side effects can be treated with prostate surgery.
Also, depending on prostate enlargement; Prostate surgery should also be planned in patients with urinary bladder stones, recurrent bleeding from the urinary tract, frequent urinary tract inflammation and no urination.
Prostate surgery method to determine the patient’s age, drugs used, additional diseases and prostate size are taken into account.
Methods used to treat prostate enlargement include:
- Medical Treatment
- Prostate Surgery
- Classical Surgical Methods
- Laser Surgical Methods
Prostate medications can be used to treat prostate enlargement. There are some side effects of these drugs that each drug uses. Also, prostate surgery was observed in some of the patients who started drug treatment due to insufficient drug treatment.
Open Prostatectomy
Prostate size of 100 gr. Open prostate surgery can be performed in patients with or above. In this surgery, the patient’s skin and subcutaneous tissues together with the bladder are opened and the prostate is removed with the help of a finger.
Because of the high bleeding rates during this operation, blood support is often required. After the procedure, the patient should stay at least 1 week probed. Also, the length of the hospital stay is longer than other methods.
With the introduction of laser in urology, surgical operations were started using the laser in prostate surgery.