What is Rheumatism?
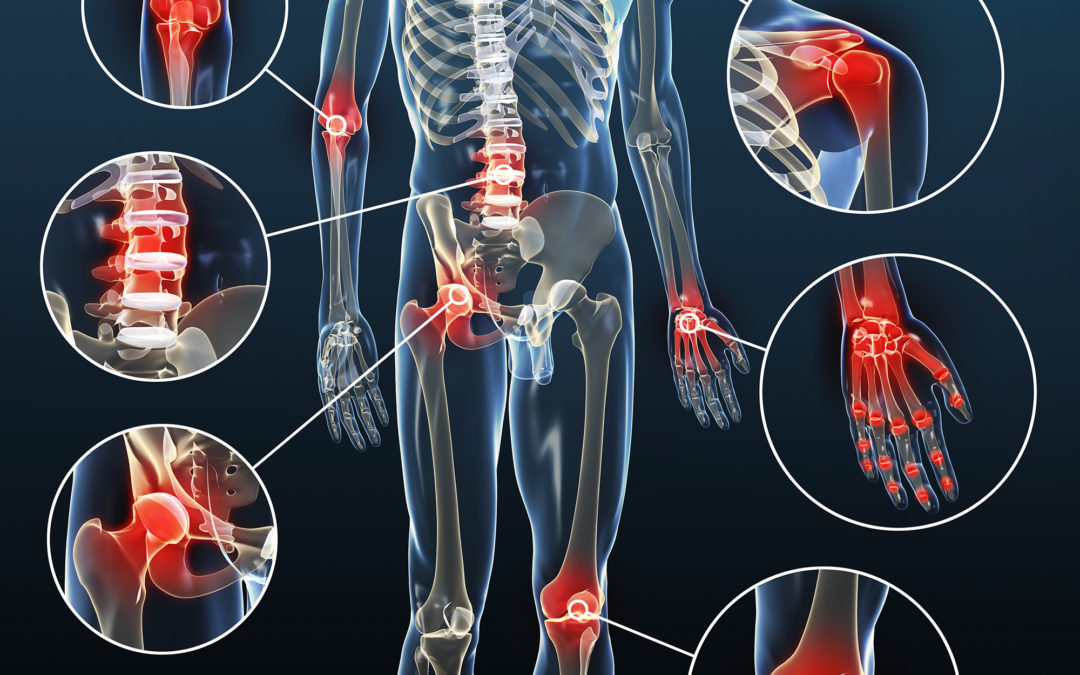
Rheumatism is derived from the Greek word “Rheuma” which means “flow”. Rheumatism is a general term used to describe dozens of diseases resulting from a disorder in the autoimmune system. Although rheumatic diseases are generally seen in the tissues that connect or support organs in the joints, muscles, they may occur in any part of the body.
Causes Rheumatism?
These diseases are caused by the immune system attacking healthy tissues instead of attacking germs, bacteria or viruses. As seen in gout, uric acid crystals (urine crystals) can also cause rheumatic disorders.
It is important to understand the main types of rheumatism and to know why they originate, both to prevent their formation and to treat them.
Symptoms of Rheumatism
Symptoms of rheumatism include;

- Muscle weakness,
- Muscle pain,
- Back and low back pain,
- Skin rashes,
- Nail changes,
- Skin hardness,
- Tear reduction,
- Dry mouth,
- Redness in the eyes,
- The sudden decrease in vision and loss,
- Prolonged high fever,
- Fading of the fingers,
- Respiratory symptoms (shortness of breath, dry cough, bloody sputum, etc.).
Same time;
- Complaints of the digestive system,
- The decrease in renal function,
- Neurological symptoms (paralysis, changes in consciousness, etc.)
- Adverse events in the heart and circulatory system (formation of clots in the veins, loss of pulse, etc.) are also symptoms of rheumatic diseases.
How is Rheumatism Diagnosed?
Diagnosis of inflammatory rheumatism can be a bit difficult. Your doctor will need to look at multiple test results at the same time to confirm clinical findings.
Your doctor will first ask for your symptoms and medical history. It will also physically examine your joints. Physical examination examines the joints for redness and swelling. Muscle strength is tested, sensitivity is checked. Check for temperature and extreme sensitivity.
Rheumatism Treatment
Although there is no definitive cure for rheumatism, treatment usually aims to suppress symptoms and prevent the disease from progressing to other organs. Various types of drugs are prescribed to treat rheumatic diseases. Some medications can only treat symptoms such as pain and inflammation, while others may alter the course of the disease. Cortisone is a frequently used, sometimes life-saving drug for the treatment of rheumatism. Rheumatism drugs must be used under the supervision of a doctor and left under the control of a doctor.
Exercise is also very good for rheumatic diseases. It is very important for resolving spasm in muscle pain to provide the flexibility of joint and spine with limited movement.
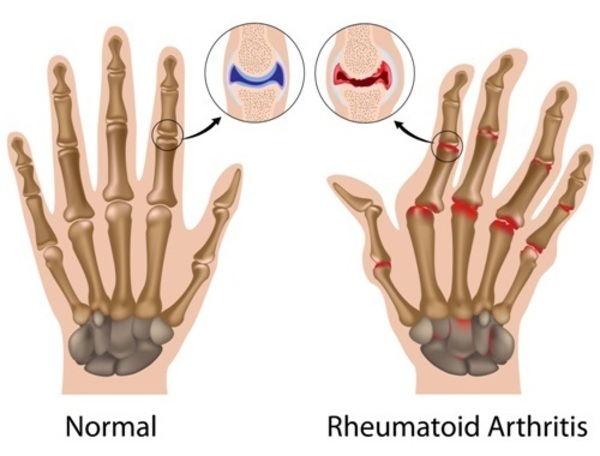
Rheumatoid Arthritis
What is Rheumatoid Arthritis?
Rheumatoid arthritis is a common form of joint inflammation and causes inflammation of the inner membrane (synovium) and/or other internal organs. The joint line becomes thicker and may cause heat in the joints, swelling and pain. Rheumatoid arthritis is a chronic disease that lasts for years. It affects many different joints in the body. It damages the cartilage, bone and joint structures.
The cause of rheumatoid arthritis is not yet known and the disease varies from person to person. It can affect everyone, including children and the elderly. However, the disease usually begins in the young and middle age. Among patients with rheumatoid arthritis, the ratio of men to women is 3/1. 2/3 of the patients are female. The disease can be seen in all races and every part of the world.
Causes Rheumatoid Arthritis?
When the immune system is functioning properly, the body defence fights against bacteria, viruses and other foreign cells. In rheumatoid arthritis, the immune system does not work properly and the body attacks its joints and other organs. In rheumatoid arthritis, inflammation cells (white blood cells, white blood cells) move from the blood to the joint tissues and attack the joints. Joint fluid increases and swelling occurs in the joint. Inflammatory cells in the joint tissue affect the joint and cause damage.
Can Infections Cause Rheumatoid Arthritis?
Many scientists and doctors believe that rheumatoid arthritis is triggered by infection. But for now, there is no proof. Rheumatoid arthritis is not contagious. A previous infection may lead to the onset of RA.
The Role of Genes:
Rheumatoid arthritis does not pass from parents to children. Instead, genes that predispose to the development of rheumatoid arthritis can be passed on to children. Children develop a predisposition to RA.
What Are The Symptoms of Rheumatoid Arthritis?
- Joint pain and stiffness, especially in the morning
- Swelling of the joints, flushing and heat increase
- Deformity of the joint
- Mild fever, exhaustion
- Anorexia
- Anaemia
- Small tubers under the skin are among the most common symptoms.
How is Rheumatoid Arthritis Diagnosed?
Early diagnosis and treatment are very important as irreversible joint damage and internal organ involvement may occur.
Patients suffering from joint swelling should consult a physician with suspicion of inflamed joint rheumatism.
There are internationally accepted criteria for the diagnosis and regulation of treatment.
Clinical findings, blood tests and radiological findings of the patient are taken into consideration when making the diagnosis. Patients who meet the diagnostic criteria should be treated as early as possible.
Treatment of Rheumatoid Arthritis
Treatment is based on the severity of the disease.
The treatment aims to reduce the patient’s complaints and prevent joint damage. The patient should be followed up regularly with clinical and laboratory findings after treatment is started.
Depending on the condition of the disease, arrangements should be made in the treatment of drugs, treatment should be started and stopped by the physician. In addition to drug treatment, physical therapy agents may be added to the treatment according to the stage of the disease, the general condition of the patient, and the extent of joint involvement.
Individual exercise therapy appropriate to the disease and the patient’s condition should be arranged.
Osteoarthritis (Calcification)
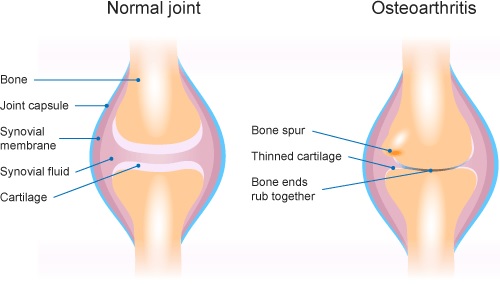
What is Osteoarthritis?
Osteoarthritis, a degenerative joint disease, is commonly known as calcification. It is the most common joint disease in people over 50 years of age. Osteoarthritis can affect any joint in the body. The most commonly affected joints are the hands, hips, knees and spine.
In osteoarthritis, joint cartilage deterioration occurs. As a result, changes occur in the bone tissue under the articular cartilage. Bone growth and protrusions on the joint edge disrupt the normal structure of the joints, causing limitation of movement and pain.
Why Osteoarthritis Occurs?
It is not clear why some joints are affected more. However, some factors increase the risk of developing osteoarthritis. These:
Age: osteoarthritis is a disease of middle and advanced age. It is rare to occur before the age of 40. Ageing changes in the articular cartilage and consequently decreases its endurance. Therefore, the incidence of osteoarthritis increases with age. Gender: Women are more likely to develop osteoarthritis, but the cause is unknown.
Hereditary factors: The substances in the cartilage content are determined as hereditary. Therefore, it is now known that hereditary factors play a role, especially in hand osteoarthritis.
Wear and wear (mechanical factors): Repetitive minor traumas over the years disrupt the load-bearing ability of the joint and cause cartilage destruction leading to osteoarthritis.
Other diseases affecting bone and joint: Gout, rheumatoid arthritis, diabetic neuropathy, Paget’s disease, septic arthritis and congenital hip dislocation increase the risk of developing osteoarthritis.
What are the Symptoms?
Osteoarthritis symptoms usually develop slowly and can be exacerbated at any time. These symptoms include:
Pain; The most common complaint. Initially, pain occurs during movement or later in the day, and relaxation occurs through listening. Joint cartilage disorders and wear may progress to pain during rest.
Seizing; occurs in the morning or after prolonged inactivity. Very short, rarely exceeds 15 minutes.
Limitation of joint movements; It may be seen in the later stages of the disease and may reach levels that disrupt the daily life functions of the person. Depending on the bone protrusions, the joint may look swollen. Although very rare, deformities (deformities) may occur.
How İs Osteoarthritis Diagnosed?
Patients with pain, stiffness and swelling of the joints should consult a doctor.
Your doctor may ask for some investigations to determine the exact cause of your complaints:
- Direct radiography (X-ray film): Joint x-ray films help in the diagnosis of osteoarthritis. However, the presence of osteoarthritis findings in X-ray films does not mean that there will be complaints in that joint, nor does it indicate the severity of the complaints.
- Blood tests: There is no blood test to diagnose osteoarthritis, but some help to differentiate osteoarthritis from other rheumatic diseases.
- Examination of joint fluid: Especially in patients with joint swelling, the examination of joint fluid may be necessary and useful in differentiating osteoarthritis from other diseases.
How is Osteoarthritis Treated?
Treatment is planned according to the stage and severity of the disease. The aim of the treatment of osteoarthritis;
- The pain relief of the patient
- Removing restrictions on movements and difficulties in activities of daily living,
- Preventing the progression of the disease.
The first step in the treatment is the education of the patient. The patient should first be made aware of the disease. Heavy exercise and excessive use of the injured joint should be avoided. With weight loss, the symptoms of osteoarthritis in overloaded joints are reduced.
Regular exercise: The muscles surrounding the joints are strengthened. This reduces the load on the joint. However, the exercise program to be applied must be arranged by your physician.
Physical therapy applications: Hot or cold applications, pain relief current treatments and deep warming treatments may be applied at the advice of your doctor.
Drug treatment: Osteoarthritis pain relief and inflammation-dispersing drugs are used during certain periods of the disease under the control of a doctor. The use of drugs that strengthen cartilage has been increasing in recent years.
Intra-articular injection: cortisone injection can be made during joint swelling if your specialist recommends it. Also, drugs that increase joint lubricity can be injected into the joint.
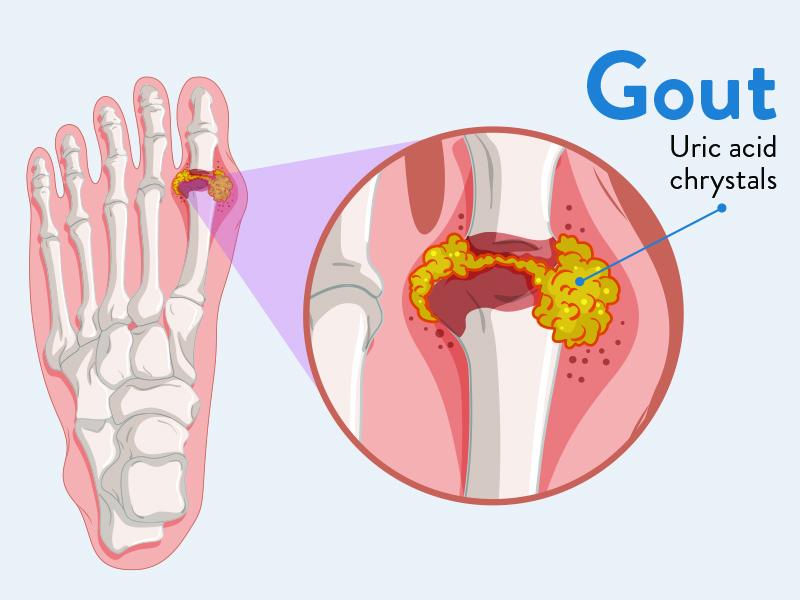
Gout
What is Gout?
Sudden joint gout is a non-microbial joint inflammation characterized by pain, redness, swelling and tenderness. It often starts on the big toe. However, knee, ankle, elbow, toe joints may also be affected. Gout is more common in men and may be associated with menopause in women. Gout, which is mostly a part of metabolic syndrome, is associated with disorders such as cholesterol, triglyceride elevation (hyperlipidemia), high blood pressure, atherosclerotic heart disease, diabetes mellitus and obesity.
Symptoms of Gout
An acute episode of gout usually begins at midnight or early in the morning with severe pain, swelling, redness, tenderness and heat in the toe or affected joint. Pain and tenderness in the joint are so severe; the person cannot step on it, move it, wear shoes or even want the quilt to touch. Pain is exacerbated in the first 12-24 hours. Occasionally, however, the joint may become less and more discomforting for several weeks.
What Causes Gout?
Gout often occurs on the big toe. However, knee, ankle, elbow, toe joints may also be affected. It may cause more serious conditions if treated. It causes damage to the joints and surrounding tissues (such as tendon, nerve compression). Gout may recur. In this case, gout attacks repeat several times a year. In advanced gout, if the condition is not treated well, urate crystals will collect under the skin and cause nodules called tofus. These nodules often accumulate on the fingers and toes, the ear canopy, the elbow, the Achilles tendon, and the soles of the feet. Tofuses are generally painless; however, it causes compression or damage to tendons and bone. Advanced gout kidney stones and urate nephropathy (impaired renal function) may be seen.
How is it diagnosed?
In the diagnosis of gout, it is important to observe mono-sodium urate crystals on a polarized light microscope when examining joint fluid. Uric acid crystals are in the form of sharp-edged crystals such as needles; gives yellow-green rifle. Blood tests can measure uric acid levels, but cannot diagnose gout. It may be normal or even low during an attack. The number of leukocytes in the joint fluid is also helpful in the diagnosis of gout.
Treatment of Gout
Treatment of gout is a two-stage treatment: attack and non-attack. The treatment aims to prevent gout attacks and complications. The blood maintains uric acid levels below 6 mg / dL.
When acute gouty arthritis develops, nonsteroidal pain and inflammation remedies (such as naproxen, diclofenac, indomethacin) should be given with gastric protectors to relieve pain and inflammation. In cases of concomitant diseases, such as underlying coronary problems or renal dysfunction, it may be preferable to use intra-articular corticosteroid injection or oral administration of low-medium dose corticosteroid.
Drugs that reduce uric acid production can be used to prevent gout complications and attacks.
Drugs that increase uric acid excretion are used. However, such drugs can cause side effects such as rash, stomach pain and kidney stones.