Coronary Artery Disease
General Promotion
Coronary artery disease (cardiovascular disease), is one of the most common heart diseases and draws attention to the vital risks posed. If it is not noticed in time and precautions are not taken, a process leading to a heart attack can be experienced. The lifestyle changed with early diagnosis reduces the risk of developing the disease.
What are the Coronary Arteries?
Your heart functions as a continuous pump to meet the blood needs of your entire body. To do this, the heart itself needs oxygen-rich blood. This blood is delivered to your heart through the coronary arteries. In short, the work of your heart is connected to the blood presented by the coronary arteries.
You may think of the coronary arteries as the first branches of the aorta, the largest vessel that distributes blood from the heart to the entire body. The left coronary artery and the right coronary artery are divided into smaller branches and feed the whole heart.
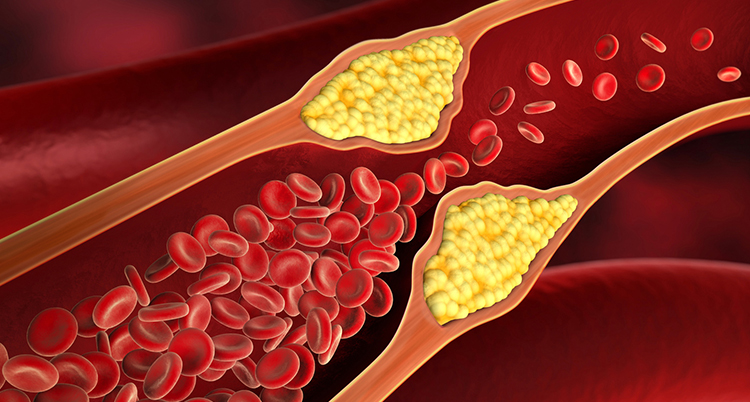
A Healthy Artery
When the inner surface of a coronary artery is healthy, blood easily flows through this vein. This allows your heart to feed on the oxygen it needs. In the event of activity, healthy arteries can easily meet the increasing need of the heart.
A Damaged Artery
The inner layer of the artery may be damaged by high cholesterol, high blood pressure or smoking. This results in plaque formation (fatty substances and calcium accumulation) in the artery wall. Therefore, blood can not flow as easily as before. This is the beginning of coronary artery disease.
A Narrowed Artery
As plaque formation increases, the artery narrows further and the blood flow to the heart muscle decreases excessively. The heart is starving for oxygen, which can cause chest pain.
A Blocked Artery
When the narrowed artery is completely obstructed by a clot, a heart attack (myocardial infarction) is passed. In the absence of oxygen-rich blood, the heart muscles in that area are permanently damaged.
Reasons
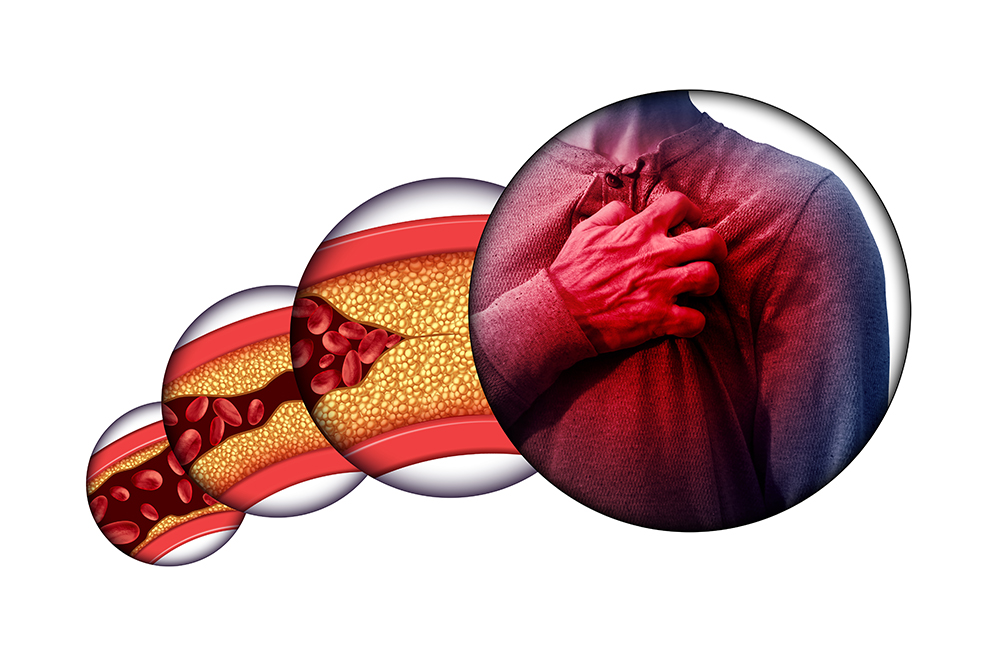
Coronary artery disease occurs as a result of the accumulation of cholesterol-containing fatty plaques on the wall of the coronary arteries, which are the vessels feeding the heart, and occlusion of the vessel within years.
The process of fat accumulation in the vessel wall is called “atherosclerosis. Progressive blockage of the cardiovascular system with atherosclerosis leads to the lack of oxygen in the heart muscle and heart failure in the long term.
Treatment Methods
Three different treatment methods are applied to patients diagnosed with cardiovascular disease. These include drug therapy, percutaneous coronary interventions and open-heart surgery. Of these, the most appropriate treatment is decided by the patient and the doctor.
Coronary Angioplasty and Stenting
Coronary angioplasty (balloon vein opening) is the process of opening local constrictions of the heart vessels through a non-surgical route.
By entering the groin arteries, the balloon in the deflated state is pushed through the veins of the heart and placed here through the lar guidewire, which is slid over this guidewire and placed in the region where the stenosis is inflated and the cardiovascular occlusion is opened.
Bypass
Coronary artery bypass surgery is another way beyond the occluded or narrowed artery, allowing the heart to be re-fed. In case of multiple occluded vessels, more than one bypass is performed. The vessels to be used for bypassing, or grafts, are taken from the chest, heart or leg and connected to the occluded coronary artery.
Minimally Invasive Methods
In endoscopic surgery, which is a minimally invasive technique, open-heart operations can be performed through small incisions in the chest area with special endoscopic devices. During the surgery, the surgical instruments are completely under the control of the surgeon.
Robotic Surgery
A robot developed for surgery operates as a result of the direction of the surgeons. The main difference of robotic surgery from endoscopic surgery is that the surgeon monitors the robot’s arms remotely and operates from a monitor.
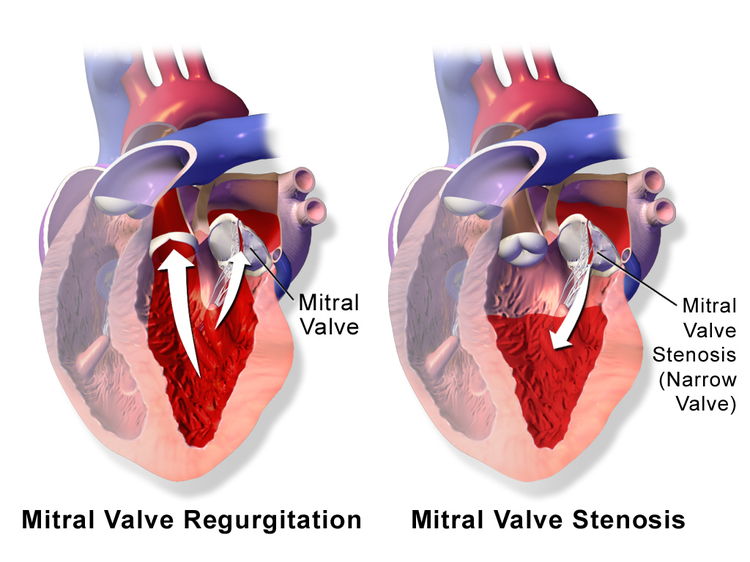
Mitral Valve Diseases
Our hearts have 4 caps. It opens and closes without any rest during the day. But when not enough is opened or closed, it causes various health problems. Moreover, at the beginning of the disease, sometimes no symptoms can be given. Many people have experienced these problems for years but do not know.
Symptoms
Complaints in valve diseases vary depending on which valve has problems. The patient may not have any complaints in the early stages of the disease. As the valve condition increases, the symptoms begin to appear.
These are generally;
- Quick fatigue,
- Weakness,
- Palpitation,
- Clogging sensation,
- Shortness of breath
It is manifested by swelling of the feet, which is an indicator of fluid collection in the body. Some valve diseases, dizziness, chest pain, even fainting complaints can be seen.
Diagnostic Methods
The diagnosis of valvular diseases can be made completely randomly by hearing a murmur while the patient is going to a doctor for any reason and resting his heart in his normal examination before these complaints start, or it can be revealed by some diagnostic methods when the complaints develop.
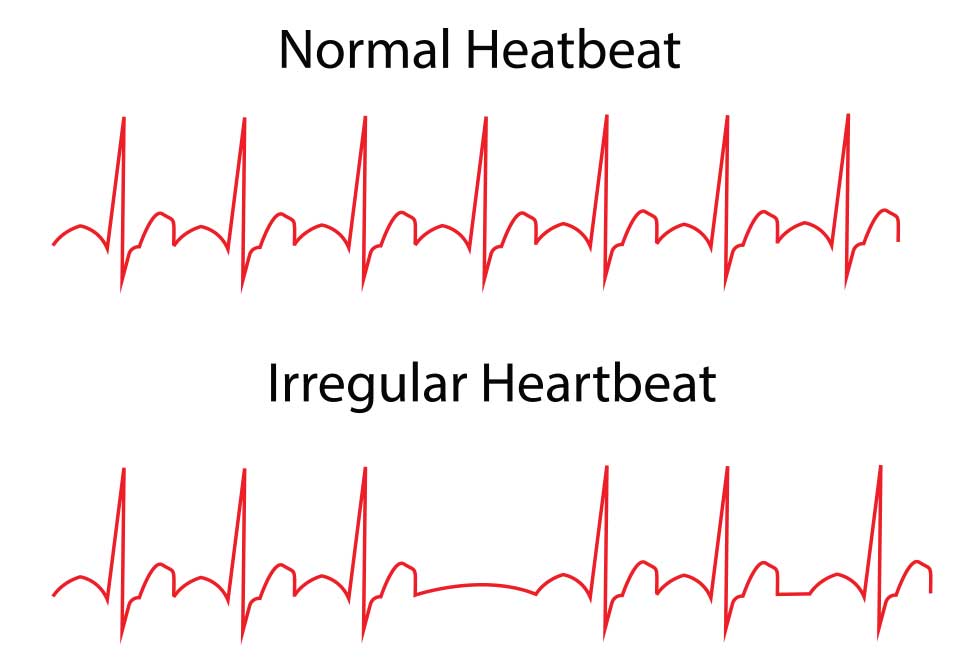
Electrocardiography (ECG)
It starts with heart rhythm. Here, the heart rate, whether it beats regularly, whether there is a problem in the vessels that feed the heart and some electrical changes specific to valve diseases are examined.
Chest X-ray
The size of the heart and the status of the lungs are evaluated.
Echocardiography
This method, which is a heart ultrasound, provides imaging with sound waves. As in the normal abdominal ultrasound of the patient at bedtime, a gel is applied to his chest and images are obtained without opening the inside of his heart.
The size of the chambers of the heart, whether the heart constricts adequately, whether the wall thickness is increased, the vascular structures and their congenital anomalies and diameters and the condition of the valves are examined. The murmurs during listening are evaluated.
Heart Catheterization
Most of the time there is no need. It’s a procedure that doesn’t put the patient to sleep. Coronary angiography method is used in cases where surgery is required and it is revealed whether there is a problem in coronary vessels.
Treatment Methods
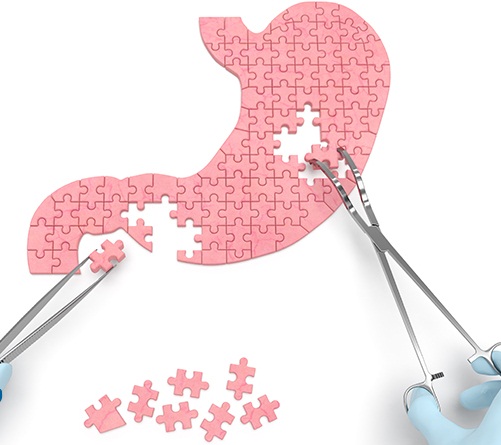
Cover Repair
The methods used in valve repair can be summarized as placing tissues supporting the valve structure, cutting and repairing the valve tissue for better closure or releasing the adhered leaflets.
Not every valve can be repaired, sometimes repair operations can be more challenging than valve replacement. While mitral valves can be repaired more frequently, aortic and pulmonary valves have to be replaced frequently.
Heart Valve Replacement
Valve diseases are most commonly treated by valve replacement surgery. During this operation, the patient’s valve is removed and replaced with a mechanical or biological valve:
Bioprosthesis valves are made from bovine, porcine or human tissue. The use of blood thinners is not necessary for the use of biological valves, but the valves may be worn out in 10-15 years and surgery may be required. In this respect, they are not preferred for young patients.
Mechanical caps can be used unchanged for life, but on the one hand, it requires you to constantly take serious blood thinners.
In cases where the aortic valve needs to be replaced, alternatively, the heart valve formed from the patient’s heart membrane can be used. With this method, which is called Oz Ozaki prosedür procedure, the patient does not need to use blood thinners. Also, clotting problem on the valve, which may occur in other prosthetic valves, is generally not observed after this technique.
Transcatheter Valve Treatment
Interventional cardiologists can repair or replace valves with the aid of clips or catheters that pass through large blood vessels.
Patients with mitral valve leakage “Mitra clip” method called with a latch attached to the ends of the valve is prevented from escaping the blood back. In the Mitra clip method, patients ‘ recovery time is much shorter than patients undergoing surgery.
TAVI
The recent current valve application is transcatheter aortic valve replacement (TAVI) for aortic valves.
In this method, the catheter is inserted through the groin vein and the balloon is advanced to the level of the aortic valve which is folded and a catheter with an artificial valve is folded around, opening the valve around the balloon inflators at the valve level and inserting it into the old valve.
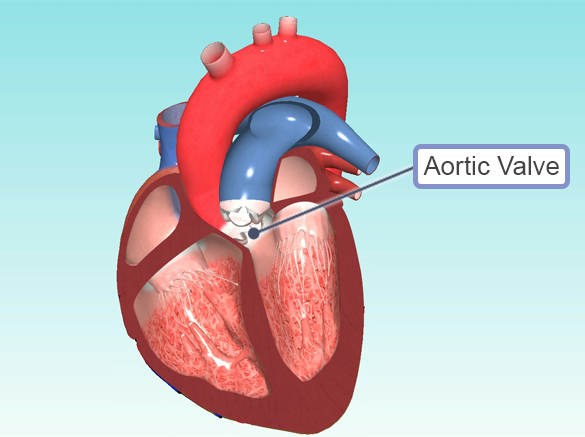
Aortic Valve Diseases
What is Aorta?
The aorta is the largest artery in our body and comes out of the left heart. The aorta is found in the lungs at the point where the oxygen-rich blood is pumped from the heart to the body tissues. This vessel, which is located in the centre of the blood circulation, pumps 5 litres of blood per minute in adults.
The aorta consists of four parts: ascending aorta, arch aorta, descending aorta and abdominal aorta. The abdominal aorta is the name given to the abdominal part of the vessel. Symptoms of aortic vascular rupture vary according to the vascular part in which the rupture occurs. Tears in areas closer to the heart present with more severe symptoms that can be fatal.
Aortic Valve Stenosis
The aortic valve is the valve between the left ventricle of the heart and the aortic vein, the largest vessel that emanates from the left ventricle and feeds the entire body.
The aortic valve has 3 petals. Sometimes it may have 2 leaves. Aortic strictures usually do not show symptoms for a long time. The first symptom is fatigue with effort.
If the aortic valve area falls below a certain value, the patient’s complaints begin. In patients with advanced aortic valve stenosis, chest pain, dizziness, fainting are seen and if not treated immediately after this stage, the patient’s life-threat is very high.
Severe Aortic Stenosis
The aortic valve is calcified and deformed, resulting in a severe contraction of the aortic valve that cannot be opened. This means that the heart forces the blood to pass through a very narrow cap as it pumps the whole body. Thus, the heart muscle remains under a greater strain and strain. This may cause the heart muscle to thicken over time and become weaker at a later stage.
Causes Aortic Stenosis?
It often develops as a result of age-related aortic valve wear and lime deposits and narrowing of the valve and restricting its movement. Having undergone rheumatic fever, radiotherapy facilitates the development of high cholesterol disease.
What are the Symptoms of a Patient With Aortic Stenosis?
- Chest pain,
- Squeezing in the chest,
- Feeling bad and fainting after strenuous work,
- Imbalance,
- Weakness,
- Shortness of breath,
How is Aortic Stenosis Diagnosed?
In the examination performed because of the patient’s complaints; The physician can hear a murmur in the heart and pre-tests, followed by echocardiography and, if necessary, cardiac catheterization and angiography.
How Is Aortic Stenosis Treated?
It is not possible to correct the calcified stenosis of the aortic valve over the years with medication. However, secondary to aortic valve disease, heart failure, rhythm disturbance, clot formation assisted medications for risk.
Treatment of aortic stenosis; surgery and catheter.
Surgical Treatment of Aortic Stenosis
Most of the heart valve operations are performed for aortic stenosis. Surgical treatment of aortic valve has been the treatment of choice for more than 40 years. This method; open-heart surgery is the replacement of the patient and calcified valve with a metal or biological tissue valve. Biological tissue valves are more preferred in elderly patients.
Is Aortic Prosthetic Valve Surgery Risky?
Normally, there is a 1% risk of life in this low-risk group and patients under the age of 70. This rate is reported as 4% when the advanced age group and all surgical patients are evaluated together.
What is the” TAVI ” catheter method and the aortic valve Placement Method?
TAVI (Aortic Valve Insertion with Catheter Method), which was developed as a new treatment method in patients with a high risk of open-heart surgery due to concomitant diseases, has been used worldwide after 2005.
Aortic Aneurysm
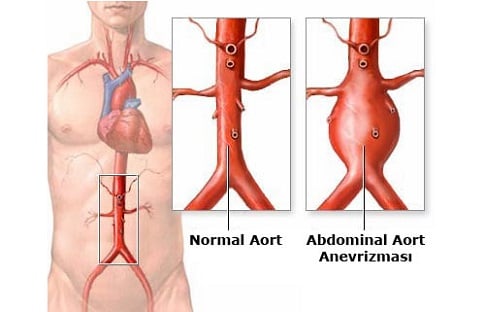
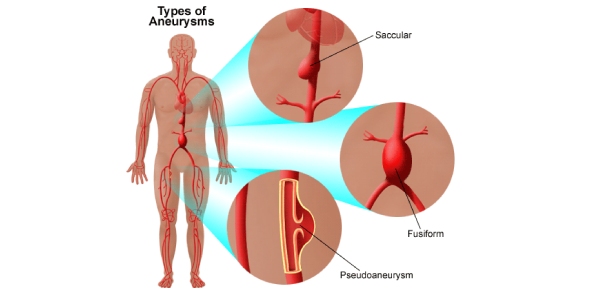
Aortic aneurysm, in its simplest terms, can be described as a kind of ballooning in an artery that leads to a 50% greater dilation of the vessel diameter than normal.
Aneurysms can be caused by very different causes depending on where they occur. Generally, high blood pressure, calcification, some infections and connective tissue diseases are among the causes of the aneurysm. In some group of aneurysms, genetic factors have a large impact. An example of such aneurysms is the lack of normal strength of the vessel wall structure resulting from chromosomal defects.
What are the Causes of Aortic Aneurysm?
1- Degeneration due to high blood pressure: It is not possible to say that high blood pressure alone is effective in the formation of an aneurysm. Many people with high blood pressure do not develop an aneurysm. However, the available data show that a significant proportion of patients with aneurysm suffer from high blood pressure.
2- Structural reactions that occur in the vessel wall, which we call degeneration and inflammation.
3- Genetic disorders due to the weakness of the vascular wall: We can show connective tissue diseases such as structural diseases such as Marfan.
4- Smoking: It is a scientific fact that smoking is directly related to the development of an aneurysm, especially beneath the renal vessels. The connection of smoking to aneurysms in the abdomen is very strong.
5- Age: Age has an important role in the formation of an aneurysm. Aneurysms, especially those occurring in the abdomen, are often seen over the age of 65 years. Aneurysms are usually problems that occur at an advanced age if the person has no connective tissue disease.
What are the Symptoms of Aortic Aneurysm?
Aneurysms usually do not give any prior symptoms, but sometimes they may be felt by different findings depending on their location. The first sign of aortic aneurysms in the abdomen, if not screened, maybe aortic rupture. For example, a persistent and uncomfortable pain that spreads through the abdomen to the waist, or a tremor that can be seen from the outside in the abdomen, maybe like feeling a ball in the abdomen when the patient puts his or her hand on it.
Aneurysms in the chest can only show chest pain or chest pain that hits the back, and even if the aneurysm is in the descending vessels of the back, it can even cause hoarseness.
How is Aortic Aneurysm Diagnosed?
With the development of medical technologies, it is now very easy to diagnose an aneurysm. After a physical examination, the diagnosis of aneurysms within the abdomen can be made, especially in weak patients. But of course, this cannot be regarded as a definite conclusion. According to the point of the aneurysm, in the aorta within the chest, X-ray can be used as the initial stage of diagnosis.
Only the x-ray film shows enlargement of the aorta. The most commonly used diagnostic method is ultrasound that works with sound waves. The aneurysm can be diagnosed with this device called ‘echocardiography’ when used in the heart and ‘abdominal ultrasound’ when used in the abdomen. According to the results of the ultrasound, further examinations can be performed. In these examinations, it is possible to clarify the diagnosis by tomographic evaluation, MRI and sometimes angiography.
How is Aortic Aneurysm Treated?
The most important data for the treatment decision is the size and location of the aneurysm. Different treatment methods are applied to the aneurysm according to the location and size. Location, size, whether the patient has any complaints affect the form of treatment.
If the aneurysm in the aorta has reached a diameter of 5.5 or six inches and the patient has no other connective tissue disease, it falls within the limit of treatment or interventional treatment. Aneurysms located in the abdomen are usually treated from 5.5 cm. Aneurysm developing on the aorta descending from the back to the back should be treated when the vessel reaches six centimetres in diameter.
Two treatment modalities are used for aneurysms that are at the limit of intervention.
1-Endovascular Method:
Without open surgery, it is applied by placing and closing the catheters that are placed in the vein and the grafts that we call stents on them.
Endovascular procedures, in which stents are inserted through the groin or intravenous, are frequently used especially in the last 10 years. Because endovascular procedures provide significant advantages especially in certain areas compared to open surgery.
2-Open surgical procedures:
Compared to endovascular procedures, they are large operations. Although open surgical procedures are now performed with smaller incisions, open surgery is perceived as large operations compared to endovascular procedures. The aim is to eliminate the diseased aneurysm and replace the artificial aneurysm. Since there is no other large vessel in the body, such as the aorta, the artificial vessel is forced. Aneurysms are disabled using polyester, PTF, Dakon-style grafts.
Atrial Septal Defect (ASD)
It is the name given to the opening of the wall between the atria of the heart.
Therefore, some of the clean blood passes to the right heart. Depending on the increased blood supply to the lung, it can cause damage to the lungs and heart, causing growth over the years.
How is Atrial Septal Defect (ASD) Diagnosed?
It usually does not show any symptoms for many years. There were even cases where the diagnosis could not be made until the age of 30-60 in people who did not go to a doctor.
This disease, but for another reason when going to the doctor, the heart murmur and heard some additional sounds or x-ray of the heart size is suspected.
How is Atrial Septal Defect (ASD) Treatment Done?
In the treatment of atrial septal defect (ASD), the size of the hole determines the time of treatment. The openings that do not close automatically and which may cause a pressure increase in the pulmonary artery is usually closed at the age of 3-6 years, ie before the child starts school.
There is usually no problem during and after surgery. There is a scar in the middle of the chest. There are also different surgical options to make this permissionless common. Catheter closure is also used in some patients.
What are the Things to do in Patients With Atrial Septal Defect (ASD)?
Children with atrial septal defect (ASD) generally do not require preventive treatment against endocarditis (inflammation of the inner layer of the heart) prior to certain interventions, such as surgery, circumcision, tooth extraction and filling, in the American Society of Cardiology’s latest recommendation booklet, if there is no additional heart disease.
However, it is recommended that they receive preventive treatment for the first 6 months after surgery or catheter treatment. Patients should be under the supervision of a doctor at intervals of about 1 year to prevent unexpected complications. This also applies to patients who have undergone surgery, more often than not.
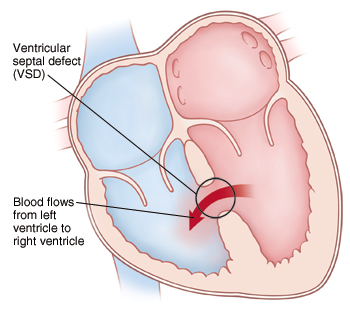
Ventricular Septal Defect (VSD)
What is Ventricular Septal Defect (VSD)?
The heart is anatomically composed of four chambers, two atria and two ventricles. A ventricular septal defect in the opening due to a congenital defect in the wall that prevents the passage of blood between the hearts.
Therefore, some of the clean blood in the left atrium passes to the right heart. Blood pressure is high in the left atrium, and high pressure passes through the right atrium. It may cause damage to lung vessels and heart muscle due to the increase of blood to the lung over the years.
Signs and Symptoms of Ventricular Septal Defect
- VSD, which usually does not murmur in the first days of life, starts to murmur while resting with a stethoscope when the baby is 1-2 months old.
- If the VSD is small and the location is not in a dangerous area in the ventricular compartment, it only murmurs but does not cause symptoms; the baby does not cause any discomfort and often closes automatically.
- Large and medium-sized VSDs show symptoms such as loss of appetite, growth retardation, shortness of breath over time, frequent breathing, difficulty feeding, excessive sweating while feeding.
- These symptoms are considered as an indication that VSD does not close spontaneously and will require surgical treatment. In these cases, the operation is usually performed in the first 3 months to prevent VSD from causing other complications.
How is Ventricular Septal Defect (VSD) Treated?
Small defects usually do not require treatment. However, they require preventive treatment against endocarditis (inflammation of the inner layer of the heart) before some attempts such as circumcision, tooth extraction, dental filling and surgery.
In moderate and large VSDs, the effects of increased pulmonary blood flow and heart failure can be mitigated, and supportive medication to regulate the heart’s work is examined to see if the patency becomes smaller as the child grows. In patients without improvement, this gap should be closed surgically.
For VSDs that do not close or shrink spontaneously, the appropriate time for surgical treatment is usually around 1-2 years.
The opening is closed with a patch and blood is prevented. In recent years, the closure of the medium-sized VSDs with suitable positions and diameters has been brought to the agenda without catheterization as in ASDs. Although not as common as ASD, there is the option of covering some of these defects with this method.
What Should be Done Prospectively in a Patient With Ventricular Septal Defect (VSD)?
The possibility of spontaneous closure of the opening varies according to the location, size and nature of the defect, but is as high as 70-80%. However, some openings may cause other problems when closing (such as anatomical and functional impairment of the valves). Therefore, the patient should be under regular control.
In patients who are small or shrunk over time but not completely closed and do not require surgical treatment, they require preventive treatment against endocarditis (inflammation of the inner layer of the heart) before some procedures such as surgery, circumcision, tooth extraction, tooth filling.
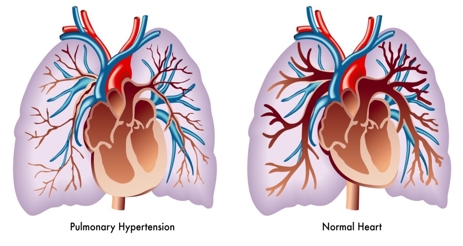
Hypertensive Heart Disease
The term hypertensive heart disease is used for heart problems caused by high blood pressure.
This is not a single disease, but rather a series of different heart diseases that result from the same thing, that is, the heart’s working under increased pressure. Hypertensive heart disease includes and other conditions: heart failure, heart muscle thickening, and coronary artery disease. For example, coronary heart disease occurs when high blood pressure causes the blood vessels to supply blood and oxygen to your heart to narrow.
Hypertensive heart disease can be dangerous and is the most important cause of death from high blood pressure.
Types
In general, heart problems associated with high blood pressure are related to the arteries and muscles of the heart.
Constriction of the Arteries
Coronary arteries carry blood to your heart muscle. If high blood pressure causes blood vessels to narrow, blood flow to the heart slows down or stops. This condition is known as coronary heart disease, also known as coronary artery disease. Coronary heart disease makes it difficult for your heart to function and supply blood to your other organs.
Thickening and Growth of the Heart
High blood pressure makes it difficult for your heart to pump blood. Like other muscles in your body, doing long-term hard work causes your heart muscles to thicken and grow. This changes the way your heart works. These changes usually occur in the main pumping chamber of the heart, known as the left ventricle. This condition is called left ventricular hypertrophy.
Complications
Both coronary heart disease and left ventricular hypertrophy can lead to:
- Heart failure if your heart can’t pump enough blood to the rest of your body
- Arrhythmia if your heart beats abnormally
- Ischemic heart disease when your heart can’t get enough oxygen
- A heart attack when blood flow to the heart stops
- Sudden cardiac arrest if your heart stops working suddenly, stops breathing, and you lose consciousness
- Stroke and sudden death may also occur.
Risks
Although the main risk for hypertensive heart disease is high blood pressure, your risk increases if you are overweight or under-exercising. Smoking and eating very fatty meals and a cholesterol-rich diet can also increase your risk.
If you have a family, you are more prone to heart disease. Also, men are more likely to develop heart disease than women, at least until the age of menopause; men and post-menopausal women are at equal risk. Whether you are a man or a woman, your risk of heart disease increases as you age.
Symptoms
Symptoms vary depending on the severity of the condition and the course of the disease. You may not have any symptoms, or you may have obvious symptoms. When the blood flow through the heart is weak, the most common symptom is chest pain (Angina Pectoris).
Other symptoms include chest tightness or pressure, difficulty breathing, and fatigue. It is also common to feel pain in the neck, back, arms or shoulders. You may suffer from coughing and/or loss of appetite. Swelling of the foot or ankle can also be a sign of heart failure.
If your heart suddenly starts to increase rapidly or irregularly, you may need emergency care. If you faint or have severe chest pain, go to the emergency room immediately.
Tests and Diagnosis
Your doctor will review your medical history, perform a physical examination and perform some laboratory tests to check your kidneys, sodium, potassium and blood count. One or more of the following tests can be used to help determine the cause of your symptoms:
- An electrocardiogram monitors and records the electrical activity of your heart. The doctor will attach patches to your chest, legs and arms. The results will appear on the screen and your doctor will interpret them.
- Echocardiography takes a detailed image of your heart using ultrasound.
- A coronary angiography examines blood flow through the heart. A thin tube called a catheter is inserted through your arm or groin through an artery up and into the heart.
- An exercise test looks at how exercise affects your heart. You may be asked to ride the exercise bike or walk on a treadmill.
- A nuclear stress test examines the blood flow to the heart. This test is usually performed while you are resting and exercising.
Treatment
The treatment of hypertensive heart disease depends on the severity of your disease, your age and your medical history.
Medicine
Medications help your heart in a variety of ways. Their main goal is to prevent blood clotting, increase blood flow and lower your cholesterol. Commonly used heart disease medications include:
- Diuretics to help lower your blood pressure
- Nitrates to treat chest pain
- Statins for the treatment of high cholesterol
- Beta-blockers to lower your blood pressure and reduce the amount of oxygen used by the heart
- Aspirin to prevent blood clots
It is important to use all medicines exactly as prescribed.
Surgery and Devices
In more severe cases, you may need surgery to increase blood flow to your heart.
If help is needed to regulate the pace or rhythm of your heart, your doctor may surgically implant a battery-powered device called a pacemaker into your chest or abdomen. A pacemaker produces electrical stimulation that causes the heart muscle to contract. Implanting the pacemaker is important and useful if the electrical activity of the cardiac muscle is improperly slow or absent.
Cardioverter-defibrillators (ICDs) are implantable devices used to treat severe, life-threatening cardiac arrhythmias.
If your condition is particularly serious, you may need a heart transplant or other heart-assisting devices.
Angina Pectoris
What is Angina Pectoris?
Angina pectoris, a disease that causes insufficient feeding of the heart as a result of stenosis caused by lipid accumulation in the vessels supplying the heart, is characterized by chest pain and chest pressure. Angina pectoris, a chest pain caused by insufficient oxygen transported to the heart muscle, usually presents during exercise or during times of stress.
It also occurs when the heart is busy and needs more oxygen. Short-term pain occurs, takes about 5-10 minutes. The pain stops at rest, but the presence of pain at rest indicates a serious condition. The shape or severity of pain does not change by breathing.
What are The Types of Angina Pectoris?
There are five types:
Exercise Angina
It is also called showcase disease because it causes the patient to stop frequently during his gait.
Cold Angina
Because cold air causes a contraction in the vessels, it also occurs as a result of coronary artery involvement.
Angina of Twitter
Excessive emotion increases the oxygen demand of the heart and occurs when the coronary artery fails to adapt to this requirement.
Resting Angina
Recurrent and continuous seizures occur when there is no apparent cause.
Bed Angina
Seizures occur in the afternoon and at night. Although it is lighter than exercise angina, it lasts longer and occurs because of the sudden contraction of coronary arteries as a result of a sudden increase in blood pressure.
What Causes Angina Pectoris?
Inadequate blood flow to the heart is usually due to coronary artery disease where the coronary arteries are narrowed due to atherosclerosis (ie, fat deposits in the arterial walls) and other causes include:
- Coronary artery spasm where blood vessels suddenly contract for a short time
- Aortic stenosis with the aortic valve of the heart narrowed
- Cardiac arrhythmias (ie abnormal heart rhythms)
Rare causes of angina pectoris pain include:
- Severe anaemia that reduces blood oxygen-carrying efficiency
- Polycythemia that thickens the blood and causes blood to flow more slowly through the heart muscle.
What are the Symptoms of Angina Pectoris?
The first symptoms are usually walking, working and so on. Occurs suddenly in ordinary situations. The most typical symptoms are pain on both sides of the chest, shoulders, arms, back and lower jaw. Deep inner distress accompanies this pain. Sweating is also seen. The seizure may not recur for a few months, but it will recur if painful conditions occur.
How is Angina Pectoris Diagnosed?
- An ECG that may appear normal between attacks
- Cardiac stress test (ECG during patient exercise)
- Blood tests
- Coronary angiography (x-ray examination of blood vessels)
How is Angina Pectoris Treatment?
Lifestyle arrangements are made and treated. Controlling high blood pressure and reducing elevated blood cholesterol levels are among the preventive measures. It is also important for the person to quit smoking and to lose weight if necessary.
Angina pectoris attacks can be prevented with nitrate drugs that increase blood flow in the heart muscle. Also, the following drugs can be used:
Beta blocking agents
- Potassium channel activators
- Calcium channel blockers
- Lipid-lowering drugs
- Antiplatelet medications
Drug treatment can control the symptoms of the disease but cannot.
Heart Attack (Myocardial Infarction)
The heart, which is located in the rib cage, a little to the left of the midline of the chest, has a muscular structure. Approximately 100 thousand times a day by contracting almost 8000 litres of blood circulating organ pump weight of 340 grams in men, 300-320 grams in women. Heart valve diseases, heart muscle diseases, coronary heart diseases, inflammatory diseases of the heart and heart attack may develop due to any disorders in the heart structure.
What is Heart Attack?
Any sudden blockage in the arteries that feed the heart can cause the heart muscle to not get enough oxygen, causing damage to the heart tissue.
In the arterial walls responsible for blood flow to the heart, substances such as fat and cholesterol accumulate and form structures called plaques. Plaques multiply over time, narrowing the vein and cracks on them.
What are the Symptoms of Heart Attack?
The most common symptom of a heart attack is chest pain, which is referred to as heart pain. The pain felt behind the chest wall is a blunt pain in weight and pressure, giving the feeling of sitting on the chest. Pain that does not feel sinking does not show an increase or decrease with movement or breathing.
It can spread to the left arm, neck, shoulders, abdomen, chin and back. It usually takes about 10-15 minutes. Resting or using medication that dilates the coronary vessels will help relieve pain. Other symptoms of a heart attack include distress, dizziness, nausea, shortness of breath, fatigue, and arrhythmia. Heart pain, sometimes due to changes in constricted areas can be experienced while at rest and pain may not respond to the drug. Such longer-lasting heart pains are more dangerous than they can easily cause a heart attack.
Causes of Heart Attack
- Smoking is the most important cause of the increased risk of a heart attack. The rate of heart attacks is almost 3 times higher in men and women who smoke.
- The higher the LDL rate, which is defined as bad cholesterol in the blood, the higher the risk of having a heart attack
- Diabetes is an important disease that increases the risk of a heart attack.
- Increased blood pressure, that is, increased blood pressure, increases the risk of heart attacks by 50%.
- With age, an increase in the deterioration and damage of the vessels is observed. This also increases the risk of a heart attack.
- The estrogen hormone in women is protective against the risk of a heart attack. Therefore, men and postmenopausal women have a higher risk of a heart attack.
- Obesity increases blood vessel dysfunction, premature ageing and arteriosclerosis, increasing the risk of heart attack
- Having a history of a heart attack in the first degree relatives of the person such as mother, father and sibling increase the risk of having a heart attack.
- Elevation of substances produced in the liver such as C-reactive protein, homocysteine, fibrinogen and lipoprotein A may increase the risk of a heart attack.
Heart Attack Treatment Methods
A heart attack is an emergency and when symptoms occur, a full-fledged hospital is essential. The majority of deaths related to heart attacks occur within the first few hours after the onset of the crisis. Therefore, it is vital that the patient is diagnosed quickly and that the intervention is performed correctly. If you have a heart attack, call a relative and the hospital immediately to report your condition.
If necessary, the doctor may perform angiography to control the patient’s vessels. According to the result of angioma, the doctor determines whether there will be medication or surgical procedure.
Congestive Heart Failure
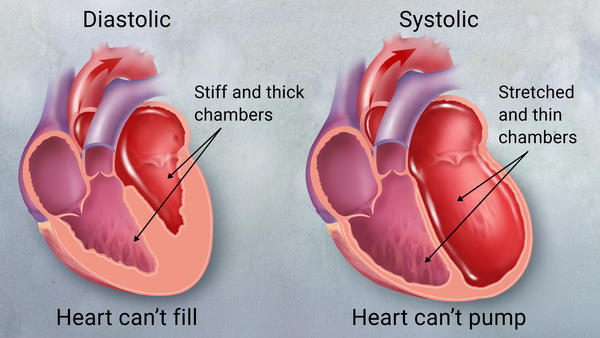
What is Congestive Heart Failure?
Congestive heart failure (CHF), sometimes referred to as heart failure, is a condition in which the heart muscle is weakened and is often unable to pump properly. The main pumping chambers (ventricles) of the heart may vary in size and thickness, cannot contract (compress) or not relax (fill) as intended. This triggers fluid retention, particularly in the lungs, legs, and abdomen.
The main factors contributing to coronary heart disease are:
- Obesity
- Unhealthy eating
- Hypertension
- Diabetes
- To smoke
- Physical inactivity.
Heart failure is more common in the elderly. The survival rate for people with this disorder depends on the severity of their condition. Treatments include medications, lifestyle changes, and (sometimes) surgery.
Symptoms of Congestive Heart Failure
As the heart fails to pump enough blood into the body, a fluid build-up occurs in the lungs and various parts of the body. This causes various symptoms. Common symptoms include:
- Shortness of breath
- Fatigue
- Swelling (oedema)
- Fast weight gain
- Cough and wheezing
- Constipation
- Swelling of the abdomen
Causes of Congestive Heart Failure
Congestive heart failure can occur for many reasons that directly or indirectly damage the heart muscle. Heart failure can be caused by several conditions, including:
- Heart attack due to coronary heart disease: a history that can lead to scarring in the heart muscles and is the most common cause of heart failure.
- High blood pressure (hypertension): high pressure in the arteries, means that the heart should continue to pump more strongly.
- Heart valve disease: damaged heart valves may allow blood to flow back or prevent forward flow.
- Congenital heart disease: there may be cardiac abnormalities such as defective valves caused by birth or abnormal communication between the heart chambers.
- Cardiomyopathy: In cardiovascular diseases called cardiomyopathy, there are structural changes such as thickening, hardening or enlarging of the heart muscle.
- Myocarditis (heart muscle inflammation): viruses or other infections can damage the heart muscle.
- Heart arrhythmia: irregular and rapid heartbeat can lead to inadequate contraction and heart failure over a long period
- Thyroid disease: Thyroid gland hormone produces too much thyroxine. This improves the functioning of the heart and can lead to heart failure.
Factors That Can Worsen Symptoms of Heart Failure
- Anaemia
- Too much salt, liquid or alcohol in the diet
- Pregnancy
- Some infections
- Kidney diseases
- Lung diseases
Congestive Heart Failure Treatment
- Medicines
- Diuretics (to remove excess fluid)
- ACE inhibitors – open blood vessels, lower blood pressure and reduce the retention of sodium and water.
- Specific beta-blockers – to slow down the heart rate and reduce it’s functioning (ACE inhibitors and beta-blockers can improve survival and reduce the likelihood of hospitalization)
- Removal of the underlying disease – for example, treatment of high blood pressure
- Lifestyle changes – such as regular mild physical activity, overweight, quit smoking, compliance with low-salt healthy eating patterns, alcohol restriction and adequate rest
- Wearing implantable cardiac devices (pacemaker)
- Surgery – to replace narrowed or leaking heart valves
- Coronary bypass surgery (in some cases)
- Heart transplantation (Final stage)
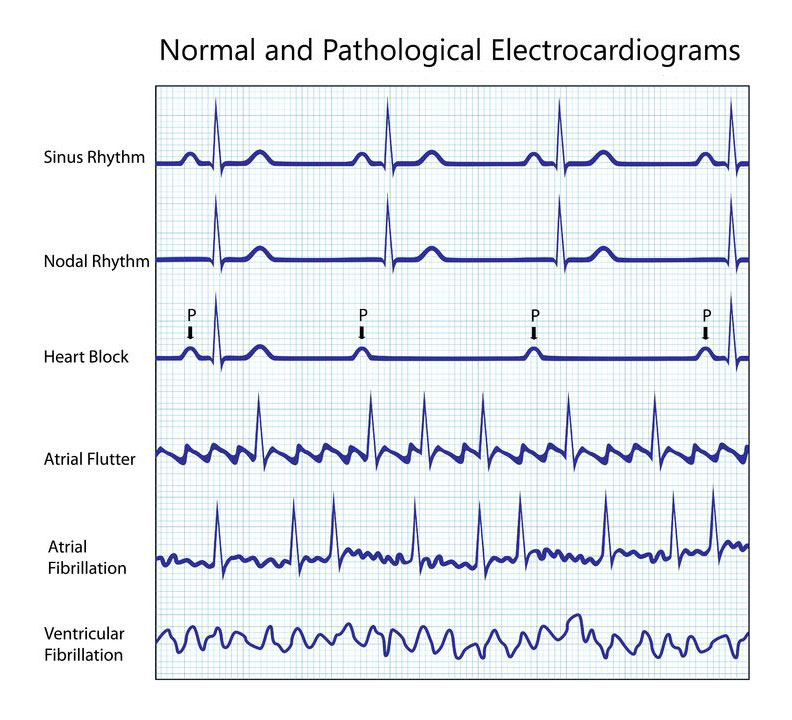
Rhythm Disorder in the Heart
Arrhythmia in the heart is a condition where the heart beats too fast, too slowly or irregularly as a result of the electrical impulses that regulate the normal beat of the heart. Rhythm disorders may occur due to problems in the heart or can be caused by external factors.
What Causes Heart Rhythm Disorder?
Rhythm disorders may occur due to many factors. Sudden heart attack, heart tissue disorder caused by a previous heart attack, coronary artery disease, high blood pressure, diabetes, smoking and alcohol consumption, drugs, stress, drugs used are the main causes of rhythm disorder.
What are the Symptoms of Heart Rhythm Disorder?
If an arrhythmia is accompanied by fainting, transient loss of vision, dizziness, feeling of dislocation of the heart, this indicates a very dangerous situation. Therefore, it is essential to consult a cardiologist without losing time, especially in such complaints. In rhythm disorders, the feeling of palpitation is prominent among the symptoms. It is among the general expressions of the patients that the heart feels as if it will come out of the chest.
Who Is At Risk for Heart Rhythm Disorder?
- Elderly and women
- Family with rhythm disorder,
- Those with cardiovascular obstruction,
- Heart valve disease,
- Those with goitre problems,
- Those with anaemia problems,
- Excessive stimulant medication intake or consumption of tea, coffee,
- Frequent and large amounts of alcohol are at risk.
Rhythm Disorders can be seen in people of all age groups. However, rhythm disorders in the heart are more likely to occur in later years and are associated with other heart diseases. Arrhythmias seen in 2% of the general population are seen in 10% of the population aged 80 years and over.
Types of Heart Rhythm Disorder that Require Emergency Response
The following conditions require immediate medical attention. They need to be treated as quickly as possible. If left untreated, they may cause damage to the heart or brain or even death.
Supraventricular arrhythmias
Supraventricular arrhythmias are arrhythmias that occur in the ventricles, ie atria. The following types of arrhythmias cause the heart to beat very quickly and require immediate intervention.
Atrial Fibrillation: This type of arrhythmia is the most common type of supraventricular arrhythmia. It is defined by irregular and rapid contraction of the atria. This type of arrhythmia can cause embolic events such as stroke and heart failure. Surgical operation is treated with other types of medical interventions and medication.
Atrial Flutter: This type of arrhythmia is very similar to atrial fibrillation. The main difference is that the heart rhythm is more regular in the atrial flutter. This type of arrhythmia is not common.
Wolff-Parkinson-White (WPW) Syndrome: This is a life-threatening type of arrhythmia and causes premature contractions of the ventricles. It occurs as a result of premature contraction of the ventricles by bypassing the atrioventricular node between the atria and ventricles by an abnormal pathway (accessory pathway).
Ventricular Arrhythmias
Ventricular arrhythmias are arrhythmias that begin in the ventricles and usually require immediate medical attention.
Ventricular Tachycardia: this type of arrhythmia is defined by the acceleration of rapid heartbeat and usually lasts for a few seconds. Ventricular arrhythmia lasting more than a few seconds requires immediate medical attention.
Ventricular Fibrillation: ventricular fibrillation is a very serious condition and can result in sudden cardiac arrest (cardiac arrest) and death. It occurs when the electrical signals in the heart become irregular. Ventricular fibrillation causes the ventricles to vibrate rather than contract so that the ventricles cannot pump blood into the body. Failure to pump blood into the body results in sudden cardiac arrest.
Bradyarrhythmias
The main symptom of brand arthritis is the slowing of heart rate. The human body needs constant blood circulation. A slowdown of the heart is a serious problem. Inadequate blood supply to the brain causes unconsciousness. It is normal for athletes and regular sportsmen to have a lower heart rate; because their hearts are strong and can pump enough blood with fewer beats. However, slowing the heart of an ordinary person can lead to a serious condition such as heart attack, chemical imbalances and slowing of the activity of the thyroid gland.
Treatment Methods
Tachycardia usually does not have a serious outcome, but it can rarely cause heart failure, stroke, and sudden death. Drugs, electrical methods or surgery are used to treat tachycardia.
Medicines
With medications, you can slow down the beating heart too quickly or completely restore the rhythm. These drugs are called antiarrhythmics. There is various rhythm regulating drugs.
Beta-blockers, calcium channel blockers and digoxin are the most commonly used agents that reduce heart rate. Antiarrhythmic drugs can be given which can completely restore the heart rhythm to normal. While these drugs are effective, they can sometimes cause serious unacceptable side effects.
Electrical Treatments
Rhythm disorders can be treated with a method called “catheter ablation” in patients where drugs are ineffective or side effects.
This procedure is performed by cardiologists who are specialists in arrhythmia called electrophysiologists at the hospital. The arrhythmia locus can be burned or frozen by detecting a piece of tissue that leads to the electrical production of the heart using a catheter.
Surgical Treatment
Some rhythm disturbances can also be treated surgically, especially for people who will be operated for another reason (eg bypass, valve surgery).
Methods Used in Arrhythmia Surgery
Maze Procedure
This treatment, which is performed with the open surgical method, is performed by opening the chest and cavities while the patient is under the support of the heart-lung machine. A highly effective treatment method.
What is Pacemaker and ICD Pacemaker?
Pacemakers are devices that consist of a combination of programmable computer chips and batteries that provide energy. They are placed in a pocket that opens under the skin, just below the collarbone on the chest wall. From here to the heart under the collarbone with the help of the needle entering the vein of the heart into the heart by placing some special cables and these cables need to be combined with the battery system.
This procedure can be done within 1-2 hours, is considered a small operation using local anaesthesia. After the operation in the operating room environment, the duration of hospital stay may vary between 1-2 days.
Who is Pacemaker?
First, it is used to relieve patients’ complaints in cases such as arrhythmias (sick sinus syndrome, AV block) that cause cardiac rhythm to slow down. There are usually single-chamber (single-cable) and two-chamber (two-cable) types.
In the last 10 years, depending on the heart failure and delay in the conduction system of the heart, three-chamber pacemakers can also be inserted for the treatment of heart failure, even if there is no slowdown in heart rate in patients with incompatibility between the left and right sides of the heart.
Pacemakers and heart atrium with the ventricle, between the two ventricles and the left ventricular wall, is trying to restore the disturbed electrical stimulation. Patients benefit from batteries with an average life of 5-6 years varies between 70 and 90 per cent.
What is ICD (Cardioverter Defibrillator)?
Pacemaker-like devices that are similar to externally programmable pacemakers. In addition to stimulating the heart in situations where the heart rate slows down, such as pacemakers, they also automatically diagnose these arrhythmias in the case of life-threatening arrhythmias and provide treatment such as shock therapy. The method of administration to the patient is very similar to the pacemaker.