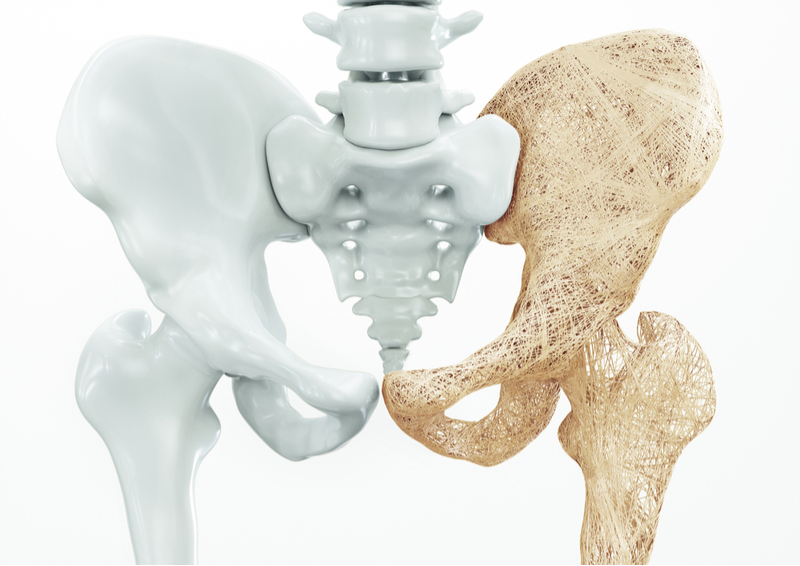
Bone Resorption (Osteoporosis)
What is Osteoporosis?
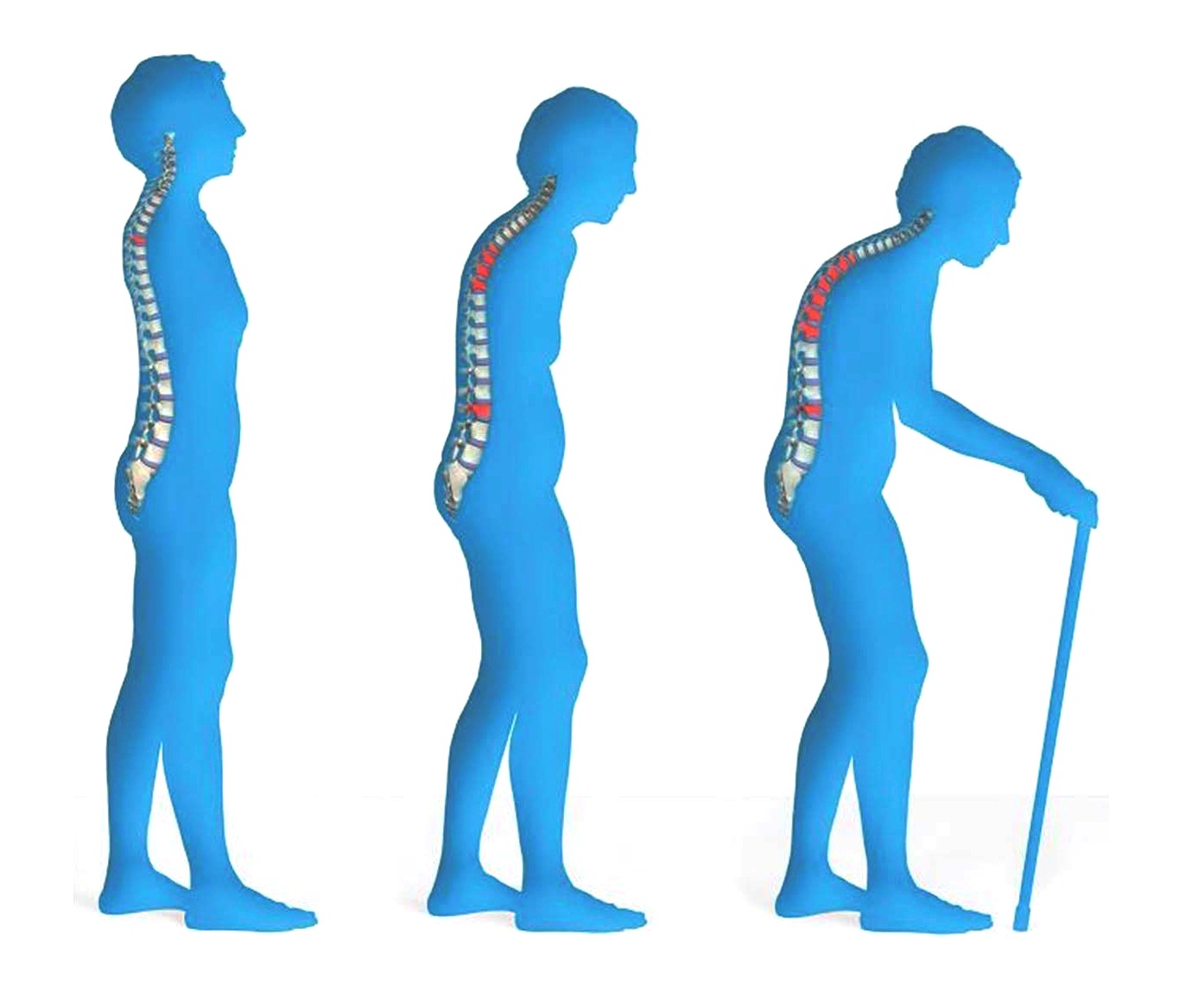
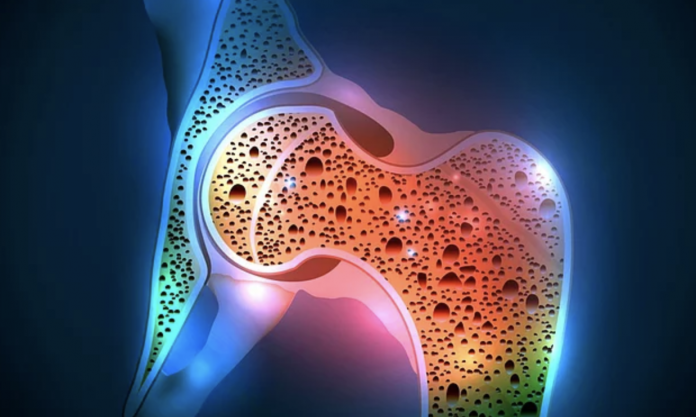
Osteoporosis in medicine; It is a disease with increased bone fragility due to deterioration of bone mass and quality.
After 35 years, the bones begin to lose the mineral (calcium) it contains. If the amount of bone formed is less than the amount of bone loss, bone loss and bone fractures occur. Women have a higher incidence after menopause than men. This is due to the decrease in estrogen hormone after menopause. It may also occur in the course of some diseases, in elderly individuals and depending on the use of certain drugs.
Osteoclasis is most commonly seen in the vertebrae, hip bone and wrists. As a result, short stature or vital spine and hip fractures may occur.
Causes
The factors that cause osteosarcoma formation are not fully understood, the effect of genetic factors or growth comes to mind. Other factors increase the risk of osteosarcoma.
Some of these factors are radioactive rays (radiotherapy) or cytostatic (poisonous cancer drugs) drugs that have previously been applied for another tumour treatment. Both can damage the structure of bone-forming cells and cause the formation of bone tumours.
Also, children and adolescents with some genetic diseases such as bilateral Retinoblastoma, Li-Fraumeni syndrome or Bloom syndrome are at high risk of developing osteosarcoma. Also, people with chronic bone disease such as Paget’s disease have a high risk of developing osteosarcoma. However, in most of the patients with osteosarcoma (90%), none of the risk factors mentioned above can be detected.
What are the Symptoms of Bone Resorption?
- Back pain
- Back and neck pain
- Length reduction
- Sloping forward and hunched posture
- Bone fractures such as wrist, hip and spine.
- In case of severe bone resorption, even simple accidents can cause fractures
- Diffuse bone pain and tenderness in the bones
- Deformations of the body due to the dissolution of bones
- Increased inactivity due to pain and fracture
How is Osteoporosis Diagnosed?
Although osteoporosis is easy to detect and treat, after the fracture occurs, it can become a socially costly situation that threatens the life of the patient and reduces the quality of life.
The diagnosis is made by clinical findings, some blood-urine tests and bone density measurement.
Individuals with diseases at risk for osteoporosis, women older than 65 years, men older than 70 years, and individuals with a history of fracture in their families should be evaluated by a physician for osteoporosis.
Can Osteoporosis be Prevented?
Genetic and environmental factors are effective in osteoporosis.
Genetic factors cannot be changed, but some environmental factors can be controlled.
It is important for individuals to exercise regularly from childhood, to feed calcium-rich and to benefit from solar energy both in the formation and maintenance of bone mass.
At the same time, reducing the consumption of cigarettes, alcohol, coffee is important in reducing the risk of osteoporosis.
How is Osteoporosis Treated?
In the treatment of osteoporosis, calcium and vitamin D are used together with certain drugs that reduce bone destruction and increase bone formation. In addition to medication, it is recommended to regulate lifestyle, exercise regularly, and use solar energy.
It has been shown that exercises against gravity, which create small loads on the bones, increase bone mass.
Special training programs such as EMS exercise program in our Physical Therapy Rehabilitation Department are among the approaches that increase bone density while decreasing fracture risk and improving quality of life in osteoporosis treatment.
What are the Surgical Treatment Methods for Osteoporosis?
If there is no fracture in patients diagnosed with osteoporosis, preventive treatment should be initiated. The main starting point in preventive treatment is to enable the patient to exercise. Brisk walks allow the bone to maintain its current strength. With activity and movement, as the person’s muscles develop, the coercive forces to the bones are reduced and thus the risk of fracture is reduced. Protective drugs can reduce and compensate for the destruction seen during osteoporosis.
In patients with fractures of the spine, the bone is surgically filled with bone cement or some organic material.
Rickets
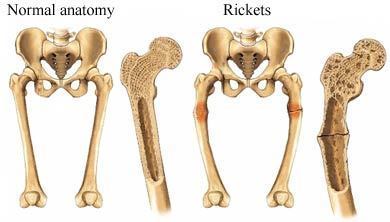
Rickets is a bone disease that develops in growing individuals due to the insufficiency of minerals such as calcium and phosphorus in the development of bones. The mineralization defect that develops after the completion of bone growth is called osteomalacia.
Rickets is a disease of many systems, mainly bone tissue. Vitamin D deficiency is the most common vitamin deficiency in our country. Since vitamin D is not absorbed sufficiently, calcium cannot be utilized sufficiently and ossification is impaired.
What are the Causes of Rickets?
- Vitamin D deficiency
- Intestinal diseases
- Kidney Diseases
- Genetic conditions
- Not seeing the sun
Some bowel diseases also cause rickets due to absorption. Vitamin D deficiency occurs due to kidneys or vitamin D deficiency occurs due to ingestion. Rickets often seen in infants is more common in infants who do not drink breast milk.
What are the Symptoms of Rickets?
Skeleton deformation:
- A strange-shaped skull (the skull is larger than the body)
- Crooked legs
- A protruding breast bone
- A curved spine
- Pelvic deformations
- Pain and tenderness in the bones of the arms, legs, pelvis or spine
- Growth disorder and short stature
- Fracture of bones
- Muscle cramps
- Tooth deformations, for example:
- Late teeth
- Tooth decay
- abscesses
- Defects in tooth structure
- Cavities between teeth
How is Rickets Detected?
Some tests are needed to detect rickets. These tests are performed for diagnosis. Diagnosis is made as a result of the tests.
Tests for detection of rickets
- Bone film
- Blood analysis
- Calcium measurement
- Phosphorus measurement
- ALP measurement
How is it Treated?
Consult your doctor for the treatment of rickets. Your doctor will ask you questions to determine if your child has rickets or possibly ask for different tests. After the diagnosis, your child should follow the prescribed medications and treatment plan.
Treatment for rickets is planned according to the underlying cause of the disease. In the treatment phase, especially vitamin D, calcium or phosphorus levels in the body should be returned to the required level.
Bone Cancer (Osteosarcoma)
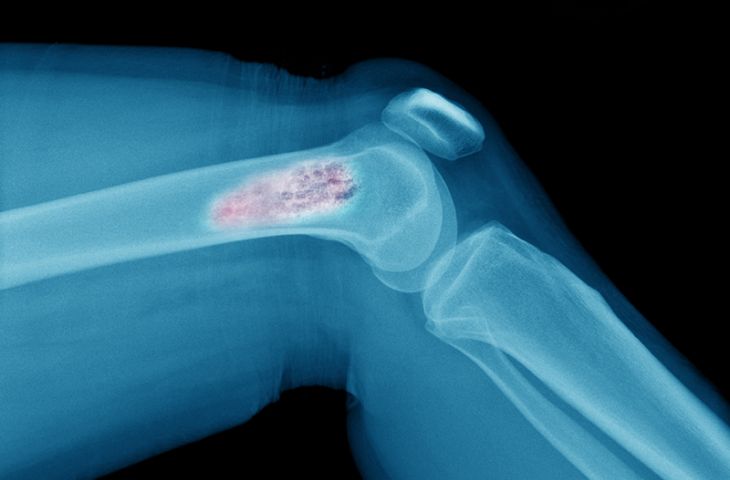
Bone cancer can start in any bone in the body but mostly affects the long bones in the pelvis, arms and legs. Bone cancers are rare and account for less than 1 per cent of all cancers. Non-cancerous bone tumours are much more common than those with cancer.
Some bone cancers occur primarily in children, while others mostly affect adults. Surgery is the most common treatment, but chemotherapy and radiation therapy can also be used.
Bone Cancer Symptoms
- Bone pain does not relieve with medication,
- If the intensity of the pain is increasing,
- If swelling and redness of the bones are noticed,
- If there are mass and stiffness in the pain area,
- Symptoms of bone cancer continue with symptoms such as loss of appetite, fatigue, fatigue, fever, disruption and rash.
Types of Bone Tumors
Malignant Tumors:
Metastatic Bone Tumors: Malignant tumours that spread to the bone from other organs. Patients often present with complaints of pain or pathological fracture that do not resolve at rest. Prostate, lung and breast cancers are the most common cancers that metastasize to the bones.
Multiple Myeloma: Multiple myelomas is the most common primary bone cancer. It is a malignant tumour of the bone marrow. It can kill 20 million people a year. It can affect any bone and is seen in patients aged 50-70 years.
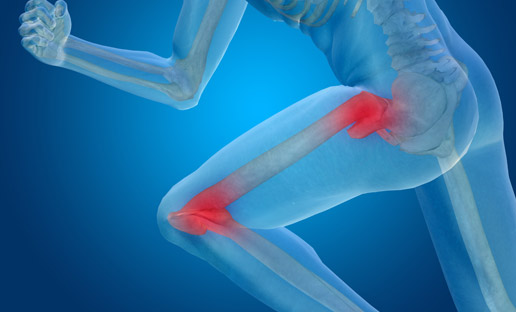
Osteosarcoma: Osteosarcoma is the second most common bone cancer. Osteosarcoma, which usually occurs in adolescence and knee region, is seen in 2-3 people per million. Rarely, it may also occur in the hip and shoulder.
Ewing’s sarcoma: Ewing’s sarcoma is commonly seen between 5 and 20 years of age; with a large soft tissue mass. It is most commonly seen in the upper and lower extremities, pelvis and ribs.
Chondrosarcoma: Chondrosarcoma is a type of bone tumour that usually occurs between the ages of 40 and 70 years with a mass in the hip region, pelvis and shoulder.
Benign Tumors:
The most common;
- Non-ossifying fibroma
- Simple bone cyst
- osteochondroma
- Giant cell tumour
- enchondroma
- Fibrous dysplasia
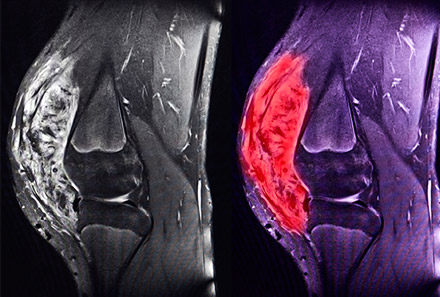
Bone Cancer Diagnosis
Imaging tests help determine the location and size of bone tumours and whether tumours have spread to other parts of the body. Recommended types of imaging tests are performed based on personal symptoms.
- Bone scan
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
- Positron emission tomography (PET)
- X-ray
- Needle or surgical biopsy
Your doctor may recommend a procedure to remove a tissue sample (biopsy) from the tumour in a laboratory test. Tests help determine whether the tissue is cancerous and the type of cancer.
Biopsy procedures used to diagnose bone cancer:
Needle Biopsy
Biopsy performed by inserting a needle into the tumour. During a needle biopsy, your doctor places a thin needle on your skin and guides the tumour. Your doctor uses the needle to remove small pieces of tissue from the tumour.
Surgical Biopsy
Surgery to remove the tissue sample. During a surgical biopsy, your doctor makes an incision on your skin and removes the entire tumour or part of it. Determining the type of biopsy you need and how to do this should be done with careful planning.
Bone Cancer Treatment
Bone cancer treatment options depend on the type of cancer you have, the stage of cancer, and your overall health. Different bone cancers respond to different treatments, your doctor will guide you in choosing the best treatment options. For example, some bone cancers are treated surgically only; some with surgery and chemotherapy; and some with surgery, chemotherapy and radiation therapy.
Surgical Operation in Bone Cancer
The surgery aims to remove the cancerous tumour. It is a procedure to remove the tumour and the surrounding healthy tissue. The surgeon can remove the lost bone from another part of your body and replace it with another bone from the bone bank or a piece of hard plastic. Bone cancers that are too large or complex on the bone may require surgery to remove all or part of an extremity (amputation). As other treatments are developed, amputation becomes less common. If amputation is required, you will be trained to learn to meet your daily needs using your new limb, possibly with an artificial limb attached.
Chemotherapy in Bone Cancer
Chemotherapy is usually performed using intravenous (intravenous) powerful anti-cancer drugs to kill cancer cells. However, this type of treatment gives better results for some forms of bone cancer than others. For example, chemotherapy is often not very effective for chondrosarcoma but plays an important role in the treatment of osteosarcoma and Ewing’s sarcoma.
Radiation Therapy in Bone Cancer
Radiation therapy uses high-power radiation, such as X-rays, to kill cancer cells. During radiation therapy, you’ll be strolling around a special machine and reaching out to a table while aiming your rays at sensitive points in your body. Radiation therapy is usually used before surgery because it can shrink the tumour and make it easier to remove.
Radiation therapy can be used for diseased tissue that cannot be removed by surgery in people with bone cancer. After surgery, it is used to kill cancer cells that may be left behind. Radiation therapy in patients with advanced bone cancer can be used to control pain and symptoms.
Chronic Myeloid Leukemia (CML)
What is Chronic Myelogenic Leukemia?
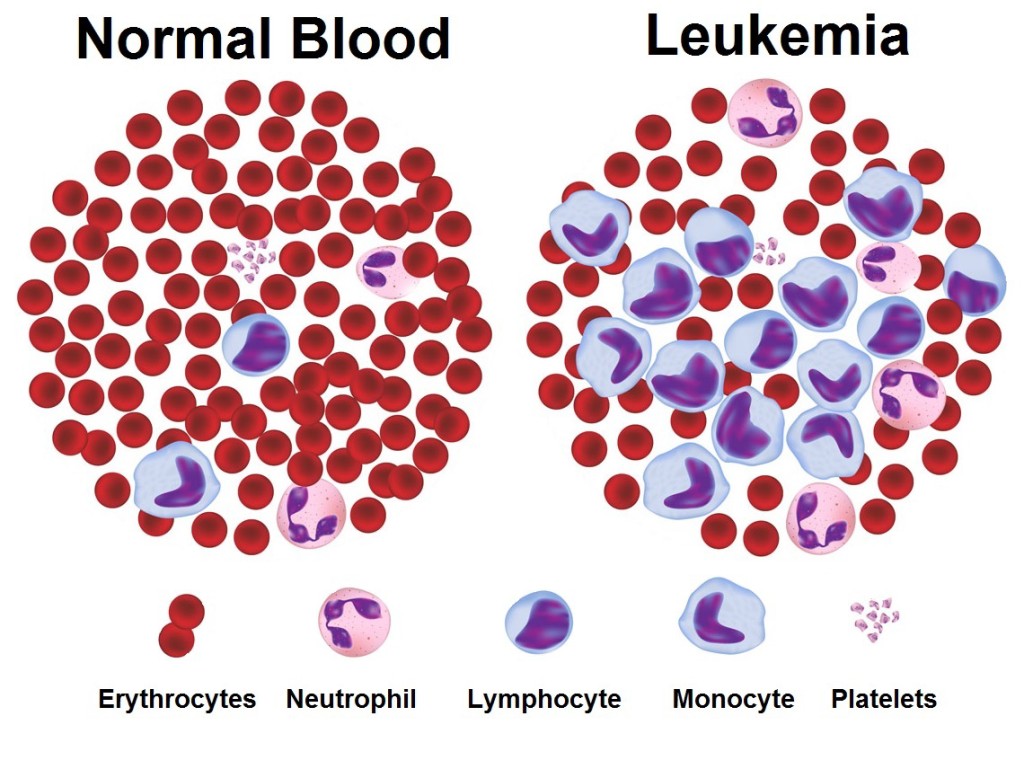
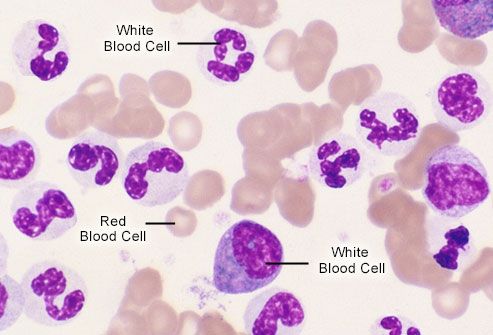
Also known as Chronic Myelogenic Leukemia or Chronic Granulocytic Leukemia. Although it can be seen at any age, it is a slow-growing cancer of blood and bone marrow that usually occurs after middle age. Chronic myeloid leukaemia (CML) is approximately one-quarter of leukaemia and 1-2 out of every 100,000 people have the disease. It is usually less severe than acute leukaemia.
CML is a blood cancer that progresses with the increase of granulocytes. These granulocytes are abnormal and do not behave like healthy white blood cells. These are called leukaemia cells. In addition to granulocytes, the cells that cause blood clotting, which we call platelets, may also increase in blood. Leukemic cells increase in bone marrow and blood, leaving no room for healthy white cells. Thus, symptoms of the disease occur. These cells also increase in other tissues, especially the spleen, and the most common finding is spleen growth.
What Causes Chronic Myeloid Leukemia?
Normal cells in our bodies contain 23 pairs of chromosomes. In most patients with CML, a structural genetic abnormality occurs on 22nd chromosomes that are not hereditary. This changed 22nd chromosomes are called the “Philadelphia chromosome“. How and why the Philadelphia chromosome is formed in blood cells is not well known, but is responsible for an uncontrolled increase in cells and prolonged survival.
A significant increase in the frequency of CML in these regions after atomic bombs suggests that radiation is one of the causes of the disease, but CML does not occur in many patients receiving radiation therapy for cancer. Also, a small amount of radiation, such as having a diagnostic X-ray film, does not adversely affect disease formation.
What are the Symptoms?
In the early stages of the disease, patients usually have no complaints. Approximately 40% of the patients are diagnosed with the presence of leukocyte levels, which are incidentally found when blood tests are performed at the hospital where they go for other reasons. With the progression of the disease;
- Fatigue in daily activities,
- Fire,
- Night sweating,
- Weight loss,
- Usually, there is a feeling of fullness, stiffness and pain under the ribs on the left side (in the spleen).
How is CML Diagnosed?
For the diagnosis of CML, bone marrow biopsy and higher-tech assays from blood are used, except for physical examination and simple blood tests. The main purpose of these high-tech assays is to show in the tests a genetic change or the results of a very common genetic structure called CML.
How is CML Treated?
The increase in leukocytes in CML is caused by the Philadelphia chromosome. A new gene called bcr-abl on this abnormal chromosome increases the activity of an enzyme (tyrosine kinase) in the patient, causing uncontrolled cell proliferation. CML is the first disease in which targeted therapies are used successfully. The drug, called Imatinib, specifically binds to cells carrying the Philadelphia chromosome, does not harm normal cells. Thus, the cells that selectively carry the Philadelphia chromosome are destroyed. Imatinib treatment provides full recovery in more than 90% of CML patients. Rarely, cases that do not respond to the drug or turn into acute leukaemia can be seen. These patients are treated with chemotherapy and stem cell transplantation.
Hip Dislocation
What is Congenital Hip Dislocation?
Although it is a serious but preventable and treatable condition, early diagnosis is very important. Congenital hip dislocation occurs when the ball on the hip bone comes out of its socket. One of the factors that cause congenital hip dislocation is the loosening of the mother’s hormones, genetic factors, cesarean delivery and the position of the baby in the womb.
Types of Hip Dislocation:
Full Dislocated Hip: The ball in the hip bone is completely out of the nest. The dislocations are replaced by applied leg movements. This is done by tilting the leg outward.
Semi Dislocated Hip: The ball in the hip bone is in the nest. However, only part of it is in an outward and upward position.
Removable Hip: As in the semi-dislocated hip, the ball in the hip bone is in the socket. However, it is easily displaced by the application of various movements.
Hip Dislocation Symptoms
Symptoms of hip dislocation are usually easily noticed during a medical examination. Newborn babies stand with their knees bent, just like in the womb. However, it is easier for newborn babies to keep their legs in a straight position, making the diagnosis easier. At the same time, the difference between the two legs, the flexibility status of the legs is different from each other and conditions such as limitation of movement play a decisive role in the diagnosis. Also, staggering of the toddler is a sign of hip dislocation.
Every newborn baby should be examined by a specialist. The examiner can refer to the orthopaedic doctor in case of any doubts and problems. At the same time, x-rays are taken in the examination of children older than 4 years.
Congenital Hip Dislocation Treatment
One of the commonly used methods in the treatment of hip dislocation is “Pavlik Bandage” or “Frejka Pillow”. With this bandage, the baby’s legs are separated from each other and pulled towards the belly. Thus, the ball in the hip bone is intended to sit in the slot. Depending on the progress in the treatment process, the bandage treatment used day and night continues for approximately 2-3 months. However, if the desired result from the bandage treatment cannot be achieved, there may be applications such as plaster treatment or suspension of the legs. Another treatment of hip dislocation is surgery. As a result of the examinations performed, surgery may be decided in infants older than 18 months.
Ewing’s Sarcoma
What is Ewing’s Sarcoma?
Ewing’s sarcoma is a rare type of cancer that occurs in the bones or soft tissue around the bones. This cancer usually begins in the pelvis, leg or arm bones, but can occur in any bone.
It may also occur less frequently in soft tissues of arms, legs, abdomen or other places.
Significant progress has been made recently in the treatment of Ewing’s sarcoma. After completion of treatment, people need to be followed for life for the potential effects of intensive chemotherapy and radiation therapy.
It is more common in young and young adults, but it can occur at any age.
Ewing’s Sarcoma Diagnosis
Typically, signs and symptoms direct parents to seek medical assistance for their children. Sometimes Ewing’s sarcoma occurs when brought to treatment with a sprain or a sports injury.
Usually, an x-ray shows a suspicious area. The doctor may then recommend one or more additional imaging tests to assess the area:
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
- Positron emission tomography (PET)
- Bone scan
- Biopsy
In the laboratory test, the doctor may suggest a procedure to remove a tissue sample (biopsy) from the tumour. The test indicates whether the tissue is cancerous and, if so, what type of cancer it is. The test also reveals the stage of cancer that helps the doctor to understand how aggressive cancer can be.
Biopsy procedures used to diagnose Ewing’s sarcoma:
Needle Biopsy
The doctor inserts a fine needle into the skin and guides the tumour. The needle is used to remove a small piece of tissue from the tumour.
Surgical Biopsy
The doctor makes an incision in the skin and removes the entire tumour (excisional biopsy) or part of the tumour (incisional biopsy).
Determining the type of biopsy required and how it should be performed is determined by careful planning by the medical team. You can ask your doctor to consult a team of specialists with extensive experience in the treatment of Ewing’s sarcoma before the biopsy.
After diagnosis, the stage of cancer should be determined. The localized Ewing sarcoma has not spread beyond its origin or near tissues. Metastatic Ewing’s sarcoma has spread to other parts of the body. Cancer stage guides treatment options.
Ewing’s Sarcoma Treatment
Over the years, significant progress has been made in the treatment of Ewing’s sarcoma.
Chemotherapy in Ewing’s Sarcoma
Chemotherapy, which uses drugs to kill cancer cells, is the priority of treatment options. Doctors recommend preoperative chemotherapy to reduce and facilitate the removal of Ewing’s sarcoma tumours.
Surgical Operation in Ewing’s Sarcoma
The goal of the surgery is to remove cancerous cells, but surgeons also perform some operations to maintain function and minimize disability. Surgery for Ewing’s sarcoma may involve removal of a small portion of the bone or removal of all limbs. The likelihood of preserving the limbs depends on several factors, such as the size, location and response to chemotherapy of the tumour.
Radiation Therapy in Ewing’s Sarcoma
Radiation therapy uses high-energy rays such as X-rays and protons to kill cancer cells. It can be used after surgery to kill the remaining cancer cells. If radiation therapy is located in a part of the body where sarcoma, surgery is not possible or with unacceptable functional consequences (such as loss of bowel or bladder function), it can be used instead of surgical operation. Radiation therapy is also used to reduce the pain caused by Ewing’s sarcoma.
Chondrosarcoma
What is chondrosarcoma?
Chondrosarcoma is a rare type of bone cancer. It develops from cartilage cells and is a category of cancers called sarcomas. Cartilage tissue is a special tissue that plays a very important role in the growth process and most bones develop from cartilage tissue. This tumour usually grows slowly and grows within the bone or on its surface.
Chondrosarcoma can be categorized as primary and secondary tumours. The primary chondrosarcoma develops from cartilage cells, while the second type develops from pre-existing benign cartilage tumours. This disease usually occurs in middle-aged and elderly people aged 50-70 and is more common in men.
Causes and Risk Factors of Chondrosarcoma:
The exact cause of this bone cancer is unknown but may be due to genetic or chromosomal factors. Chondrosarcoma is not contagious.
Knowing the risk factors of this disease can help you monitor the tumour and get the appropriate treatment. Chondrosarcoma usually develops from normal healthy cartilage cells, but may also arise from a pre-existing cartilage tumour. Here is a list of some benign tumours in which chondrosarcoma can develop!
Enchondroma:
It is a benign bone tumour that develops from cartilage cells usually seen in the hands.
Osteochondroma:
Cartilage and bone tissue are overgrowth together and usually develop from the end of a long bone.
Ollier’s Disease:
It is a group of enchondromas affecting hands.
Maffucci Syndrome:
Maffucci syndrome is a genetic disorder associated with a high rate of cancer. It affects both men and women and is characterized by bone deformities, cartilage augments.
Symptoms of Chondrosarcoma:
The symptoms of chondrosarcoma may vary from person to person depending on the size and location of the tumour. The most common symptoms are:
- Swelling on bone, swelling of joints and tenderness in affected areas and pain in normal movements
- Weak or broken bones in the affected area
- Pain worsening at night and relieving with anti-inflammatory drugs
- Pain does not relieve relaxation.
- If the tumour spreads to the lungs, it may cause breathing or bloody coughing.
- The pain gradually worsens and may last for years.
Chondrosarcoma Diagnosis:
Chondrosarcoma can be diagnosed with the necessary tests and x-rays. It also includes a physical examination of the bones to check for the presence of swelling or tenderness. Apart from these tests, the genetic history of the doctor should be examined. The tests that can be performed for the diagnosis of this tumour are given below.
Biopsy:
It is a diagnostic test that examines the tumour sample taken from the affected bone of the person. This sample is examined under a microscope to determine the type of tumour or any abnormal cells that may be present.
X-ray:
It is a diagnostic test for imaging internal tissues, bones and cartilages that use electromagnetic radiation.
Computed Tomography:
It is a method that more clearly shows internal organs, bones and cartilage tissues than X-ray.
Magnetic Resonance Imaging (MR):
It is a test that uses magnetic waves to produce internal images of organs, bones and structures.
Chondrosarcoma Treatment:
The type of treatment depends on the aggression of the tumour, the location, size and degree of cancer. The main treatment is the removal of the tumour. It will also be decided by the doctor based on the patient’s age, previous illness history and medical history.
Surgical:
Since this type of cancer usually does not respond to radiation and chemotherapy, surgery is the main form of treatment for this cancer type.
Physiotherapy:
Physical therapy helps to heal the affected area and restore its strength after surgery.
Radiation Therapy:
In this treatment, high-power X-rays are used to mark and destroy cancer cells. Reduces the risk of cancer spread to other organs. It is usually performed postoperatively.
Chemotherapy:
Chemotherapy uses anti-cancer drugs to destroy cancer cells in the body. This treatment may be necessary if cancer has spread to other parts of the body.
Tumours may recur, so the patient must visit the doctor regularly. The recovery period may vary from person to person, and emotional support from family and friends is highly necessary.
Fibrous Dysplasia
What is Fibrous Dysplasia?
Fibrous dysplasia occurs with the development of fibrous tissue in the bone. Fibrous tissue develops within the bone, replacing the bone tissue, resulting in the weakened fibrous bone. Weak bone deformities and fractures develop.
Which Bones İnvolve Fibrous Dysplasia?
Fibrosis dysplasia can occur in any bone of the body. Commonly involved bones: femur, tibia, pelvis (thigh), ribs, skull, humerus.
What are the Symptoms of Fibrous Dysplasia?
Pain and difficulty in walking due to bone deformities are common findings. Bone fractures may occur.
More severe fibrous dysplasia has the following symptoms:
- Bone pain, usually mild to moderate pain
- Swelling
- Bone deformity
- Bone fractures, especially in the arms or legs
- The curvature of leg bones
- Fibrous dysplasia can affect any bone in the body.
Diagnosis of Fibrous Dysplasia
Direct radiography, computed tomography and MRI are frequently performed for diagnosis. Bone scintigraphy may also be required. A needle biopsy can also be performed for diagnosis.
Fibrous Dysplasia Treatment
If the patient does not have complaints or deformities, the disease is only followed in the first stage. Bisphosphonate drugs used in osteoporosis are used to prevent bone loss in the development of signs and deformities. In advanced cases, fibrous dysplasia lesion is removed with surgical treatment and bone grafts are replaced.
However, the most commonly affected bones are:
- Skull
- The thigh bone (femur)
- Tibia
- Upper arm bone (humerus)
- Rib
- Pelvis
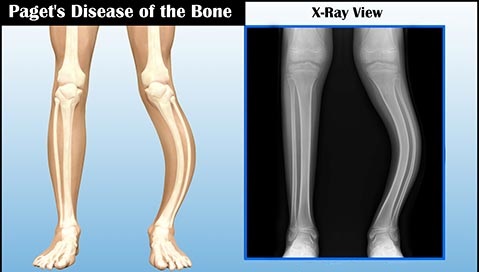
Paget’s Disease
What Causes Paget’s Disease?
The exact cause of Paget’s disease is unknown. However, both genetic and environmental factors are thought to be triggered by triggering.
1) Genetic Factors
10-15% of Paget’s disease cases are triggered by genes from the family. People who have Paget’s disease in one of their parents, siblings, are about eight times more likely to develop Paget’s disease.
2) Environmental Factors
The following diseases and conditions are thought to trigger Paget’s disease:
- Measles
- Youth disease (dog disease)
- Respiratory syncytial virus (RSV)
- Rural lifestyle
- Malnutrition
- Rickets
Paget’s Disease Treatment
1)Close Monitoring
Many cases of Paget’s disease do not require any treatment. If no symptoms are seen despite the diagnosis, regular blood tests will monitor the course of the disease and intervene if necessary.
2) Regulation of Bone Development
Bone growth can be promoted and regulated using the following drug treatments:
Bisphosphonates: The first treatment option. It controls the cells that break down the bone. In this way, the bone regeneration process is expected to return to normal. It is generally recommended to consume one tablet per day for two months. Pamidronate syringes may also be recommended.
Zoledronic Acid: A new bisphosphonate used as an alternative to risedronate and pamidronate. Used as a syringe. The effect is long-lasting. Even one syringe in two years may be enough.
Calcitonin: If your calcium level in the blood is low, the use of bisphosphonates can be dangerous; because there is a risk of further lowering. In these cases, artificial calcitonin hormone, which prevents bone destruction, may be necessary.
Painkillers: Paracetamol or ibuprofen may be recommended if bone pain is involved. In cases where these medications are inadequate, stronger painkillers will be recommended by doctors.
3) Food Supplements
Calcium is a very important component of bone development. Most Paget patients are advised to take calcium supplements regularly. Some drugs used in Paget’s disease have a risk of lowering blood calcium levels. This makes calcium supplements even more important.
4) Physical Therapy
Some medicinal products may be recommended to relieve pressure on bones affected by Paget’s disease:
- Walking stick etc. walking supports
- Orthotics used as insoles
- Corsets for spine
Some therapists may also apply the following treatments:
- Electrical waves to stimulate the nervous system (energy-based therapy)
- Exercises to increase muscle strength
- Joint therapies to maintain range of motion
5) Surgical Intervention
Surgical intervention may be necessary for serious problems such as a bone fracture. In cases of severe bone resorption, joint repair or replacement may be required. Occasionally, osteotomy (bone cutting) maybe necessary to straighten the deformed bone.