Rectal Cancer
What is Rectal Cancer?
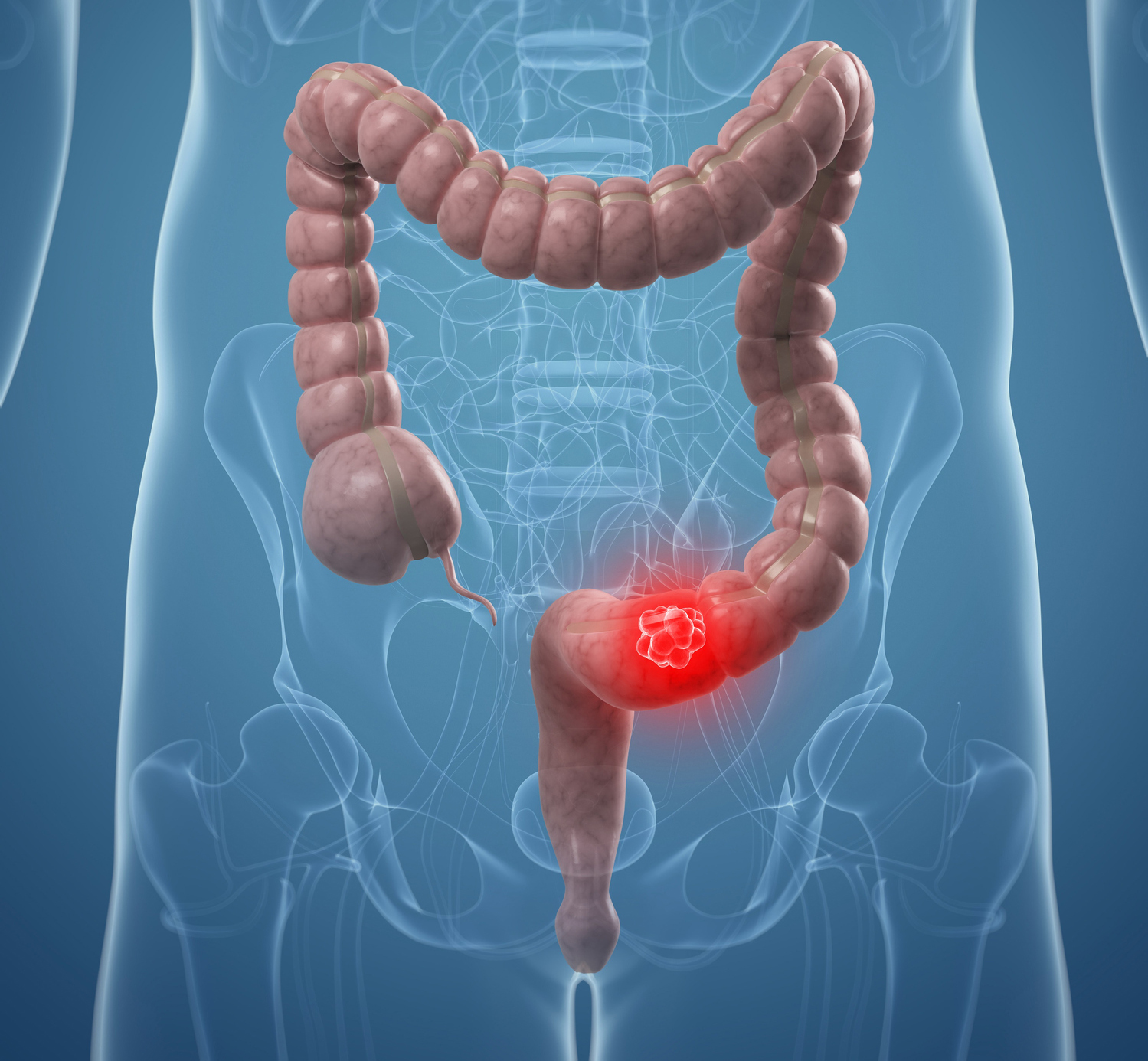
The first 12 cm portion of the large intestine, which is close to the breech, is called the rectum, and malignant tumours arising from this section are called rectum cancer. Although the incidence increases from the age of 35, it is most common after the age of 50. It is the third most common type of cancer in the Western world and the second most common cause of death. It occurs mostly from adenomatous polyps that occur in the large intestine.
Risk Factors for Rectal Cancer
- Age over 50,
- Diet, rich in fat, poor nutrition from the pulp, no consumption of raw fruits and vegetables, excessive red meat consumption, smoking,
- Family with large bowel cancer or large bowel polyps,
- Those with inflammatory bowel diseases such as ulcerative colitis and Crohn’s disease.
What are the Signs of Rectal Cancer?
- The most common symptom is a change in defecation habit. People with regular toilet habit may develop diarrhoea or constipation attacks. But the more frequent complaint is the inability to relax after performing a large ablution called tenesmus.
- Rectal bleeding is the most neglected complaint. In general, patients do not consult a doctor because of a feeling of embarrassment or because this haemorrhage is caused by haemorrhoid and this diagnosis is made at a later stage.
Apart from these two symptoms, abdominal pain, intestinal obstruction, anaemia and severe ablutions or incontinence complaints may be seen in advanced stages.
The diagnosis of a rectal tumour can be easily diagnosed by rectal examination of the rectal finger and a colonoscopy.
Treatment of Rectal Cancers
The main feature that separates the rectum from the column is the difference in its location. Therefore, unlike colon cancer, different treatment options are applied in rectal cancer. The most important criterion in the selection of the surgery is in which part of the tumour (upper, middle, lower rectum) is located. Another important selection criterion is the stage of the tumour, especially in lower rectal cancers. Therefore, clinical staging is very important in planning the appropriate treatment. In addition to endoscopy and biopsy; Computed Tomography (CT), Endorectal Ultrasonography (ERUS), Magnetic Resonance (MR) and Positron Emission Tomography (PET) are used.
Surgical Methods
Low Anterior Resection;
It is the most common method in rectal cancer surgery depending on tumour location. The intestine and lymph nodes in which the tumour is located are removed, then the end of the colon above is connected to the rectum or anal canal, which is maintained below, to maintain the intestinal continuity.
Abdominoperineal Resection (APR-Miles Method);
It is a surgical method for large tumours located near the anus and spreading to the sphincters at the end of the rectum. In this method, the rectum and breech are completely removed and the end of the colon is mouthed to the anterior abdominal wall (colostomy).
Local Excision with Transanal Endoscopic Microsurgery (TEM);
It is a method of removing the tumour with firm borders and closing the opening with special surgical instruments placed in the rectum in early-stage rectum tumours.
Chemotherapy and Radiotherapy in Rectal Cancers
Unlike the colon, rectal cancers have a higher risk of postoperative recurrence than colon cancers due to the absence of the outermost layer in the rectum wall, the higher lymphatic flow and the anatomically located within the narrow pelvis.
In advanced stage rectal tumours and selected patients, preoperative chemotherapy and radiotherapy are aimed to reduce tumour size and depth of invasion and increase tumour removability, thus minimizing the risk of locomotion.
Rectal Polyps
What are Rectal Polyps?
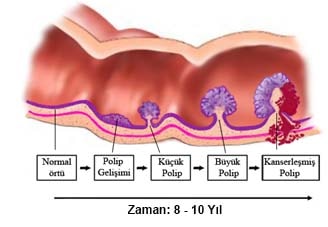
Polyps occur in approximately 20-30% of the population. And it is very common in imaging methods. These develop as a result of uncontrolled growth in the innermost layer of the intestine called the mucosa.
Polyps can be seen throughout the large intestine. However, it more often develops in the left colon, sigmoid colon, and rectum. Polyps are benign tumors. However, some types can develop into cancer over the years. More than 90% of colon and rectal cancers develop from a polyp.
What are the Symptoms of Polyps?
Many colorectal polyps do not cause any symptoms. Therefore, screening programs and imaging tests are very important.
The presence of polyps may lead to blood in the stool in some patients.
Excessive mucus production, changes in bowel habits, diarrhea and abdominal pain are other symptoms that can be seen in polyps.
How are Polyps Diagnosed?
The most common method for detecting polyps is a colonoscopy. During this day, your doctor examines your large intestine with the help of a long, flexible and lighted instrument.
If polyps are detected during the process, they are also removed. It is not possible to detect polyps by other radiological imaging methods.
Very large polyps can be imaged by chance in tomography examinations performed for other diseases. If a polyp is detected in the colonoscopy, it is necessary to repeat the colonoscopy periodically to remove or follow them.
Is it Necessary to Treat Polyps?
Since there is no visual evidence to predict whether a colorectal polyp will develop into cancer, polyps should be removed and pathological examination performed. The majority of polyps can be removed during a colonoscopy.
In large and flat base polyps, removal by colonoscopy may be difficult, insufficient and risky for bowel perforation. Therefore, some patients may require surgical treatment to remove the polyp. If rectal polyps cannot be removed by colonoscopy, the polyp can be removed by TAMIS method.
Breech Sagging (Rectal Prolapse)
Rectal prolapse is the stretching of the rectum (the last part of the large intestine is located just above the breach region) and hanging out from the breach. Faecal incontinence can often be seen by the difficulties of the sphincter muscles that serve to contract the breach.
Why Does it Occur?
Many factors are effective in the formation of rectal prolapse. Long-term changes in intestinal habits may even be seen as a late finding of a process that begins in childhood.
Although very rare, there is the genetic transmission. In many patients, loosening of the ligaments that allow the rectum to hang on the pelvis and weakness of the sphincter muscles are involved.
Occasionally, rectal prolapse is accompanied by insufficiency of the pelvic floor and incontinence or prolapse of other organs within the pelvis. It can also be seen as a result of spinal cord damage and diseases.
Is Hemorrhoidal Disease and Rectal Prolapse the Same?
Bleeding or prolapse of mucosal tissue from the rectum may be a common symptom of both diseases, but a higher level of intestinal prolapse occurs in the rectal prolapse. In hemorrhoidal disease, the breach region, called the anal canal, is sagging.
How is Rectal Prolapse Diagnosed?
Diagnosis can be made by a careful history of the physician and a complete anorectal examination. To be able to see the prolapse, in some cases, the patient is asked to push the toilet into a sitting position and prolapse is observed. In some cases, rectal prolapse may not be monitored because it remains inside.
If there is occult rectal prolapse, the diagnosis can be made by using radiology method that examines the movements of the rectum and rectum during defecation. The so-called anal manometry, which measures the pressures of the breach muscles, can show weakness in the muscles and sphincters surrounding the rectum.
How is it Treated?
The treatment of rectal prolapse is surgery. In cases where constipation and overexpression trigger rectal prolapse, simple dietary recommendations cannot control the disease after rectal prolapse develops. Many surgical methods have been described for treatment.
In the selection of techniques that can be recovered from the abdominal approach and the rectal approach, the degree of prolapse, the age and physical condition of the patient and the result of the diagnostic tests are important. Abdominal approaches can be performed by laparoscopic method.
What is the Success of Surgery?
Almost all of the patients are completely relieved or relieved to a great extent after the surgery. The success of surgery depends on many factors such as the condition of preoperative sphincters, prolapse or prolapse, and the condition of the patient.
Solitary Rectal Ulcer Syndrome
What is Solitary Rectal Ulcer Syndrome?
The last part of the large intestine that is close to the breach is called the rectum. The rectum attaches to the pelvis with muscles and ligaments. Aphthous ulcers or wounds from the rectum are called ‘solitary rectal ulcer syndrome’. Solitary rectal ulcer syndrome was first described by Cruveilhier in 1829, but its original presence was recognized in 1969 after the clinical study of Madigan and Morson.
Causes Solitary Rectal Ulcer Syndrome?
- Intussusception of the intestine into each other as a result of the veins are stretched and blood in the intestine (ischemia) and then ulcers develop.
- Irregular contraction of pelvic floor muscles (spastic pelvic floor syndrome)
- Efforts to drain faeces: removing faeces in case of chronic constipation by enema or finger.
- Breech sagging (rectal prolapse): 40% occurs.
- Radiotherapy: after irradiation of tumours in the abdominal cavity and pelvis (rectal cancer, prostate cancer, etc.)
- Stool petrification (fecaloma)
- Excessive strain
- Some migraine medications (containing ergotamine)
What are the Symptoms of Solitary Rectal Ulcer Syndrome?
- Pain in the breech
- Bleeding from the rectal
- Defecation difficulty
- Abdominal pain
- Changes in defecation habits
- Faecal complete discharge
- Slimy (mucus) discharge
- Gas or faecal incontinence
- Diarrhoea: 20% is seen.
- Team (Venezia or tenesmus): the continuous feeling of straining, but not defecation.
- No symptoms: no symptoms are seen in 25% of patients.
The mean period between the onset of symptoms and diagnosis was 5 years.
Which Diseases Can Solitary Rectal Ulcer Syndrome Mix?
- Haemorrhoids (haemorrhoids, yeast, paternal)
- Breech fracture (anal fissure)
- A breach abscess (anorectal abscess, anal abscess, perianal abscess)
- Anal cryptitis: An infection of the hair and sweat glands (4-10 pieces) which serves as a lubricant to facilitate the excretion of faeces in the breach region.
- Rectal cancer
- Breech cancer (anal cancer, anus cancer)
- Inflammatory bowel diseases (Crohn’s disease, ulcerative colitis)
How is Solitary Rectal Ulcer Syndrome Diagnosed?
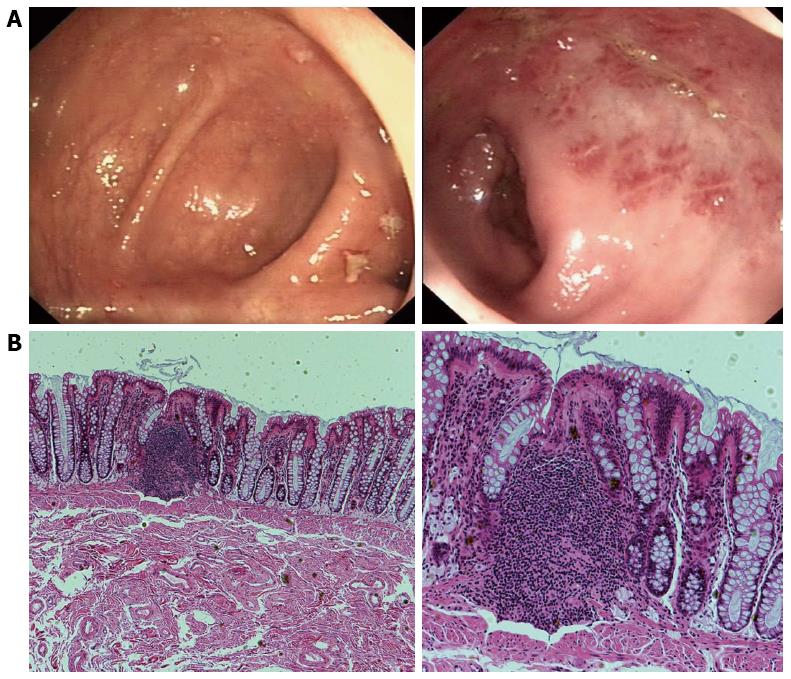
- Endoscopy: Rectoscopy (proctoscopy), sigmoidoscopy, a colonoscopy may present as redness and ulcers in 20% (mucosa) of the intestinal surface, polyps in 25%, and multiple ulcers in 30%.
- Ultrasonography: Endoscopic rectal ultrasonography (ERUS) or endoanal ultrasonography (EAUS)
- Defecography: It is the process of imaging the rectal canal (anal canal) and rectum called intestine with the breech.
- Anorectal Manometry: In 55% of the patients with solitary rectal ulcer syndrome, anorectal manometry examinations showed signs of anal dissynergy or anismus.
How is Solitary Rectal Ulcer Syndrome Treated?
- Life changes
- It is useful to get water around 2 Lt per day.
- It is beneficial to keep the amount of diet in the lift around 25-35 grams per day with fruits, vegetables and cereals.
- Regular sports: regular sports for at least 30 minutes several days a week is beneficial.
- Avoid coffee and sodas.
Drugs: Sucralfate, cortisone, mesalamine and sulfasalazine containing enemas are beneficial.
Biofeedback: Patients are trained to avoid over-strain, especially during bowel movements. The main objective is to teach patients the relaxation of pelvic floor muscles. In biofeedback treatment, the breach muscles can be strengthened by inserting a device into the breach and thus both defecation number and defecation difficulty can be corrected in 65% of the cases.
Endoscopic Treatments
- Sclerotherapy: 5% phenol, 30% hypertonic serum or 25% glucose is injected into the submucosa of the rectum by endoscopic injection.
- Laser Treatment: The ulcer site is burned endoscopically by laser.
- Fibrin Glue: The ulcer floor is endoscopically covered with fibrin glue.
Surgical Intervention:
- Rectopexy: If the patients have rectal prolapse (rectal prolapse), the rectum upward (rectopexy) is performed. In recent years, this technique has been frequently applied with laparoscopic or robotic surgery.
- Delorme Surgery: The inner part of the rectum called the mucosa is cut and then fixed with sutures.
- Stoma: Is a surgical operation of the rectum and colostomy (oral intestine of the large intestine, bowel sac, bowel bag).
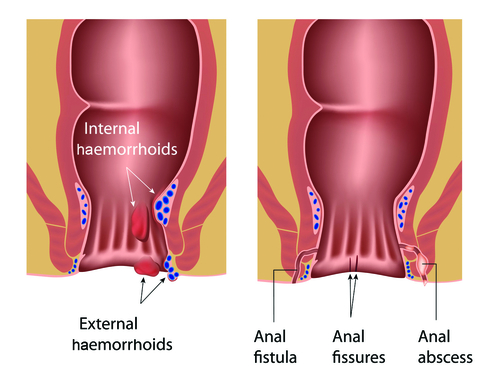
Hemorrhoid
What is Hemorrhoid?
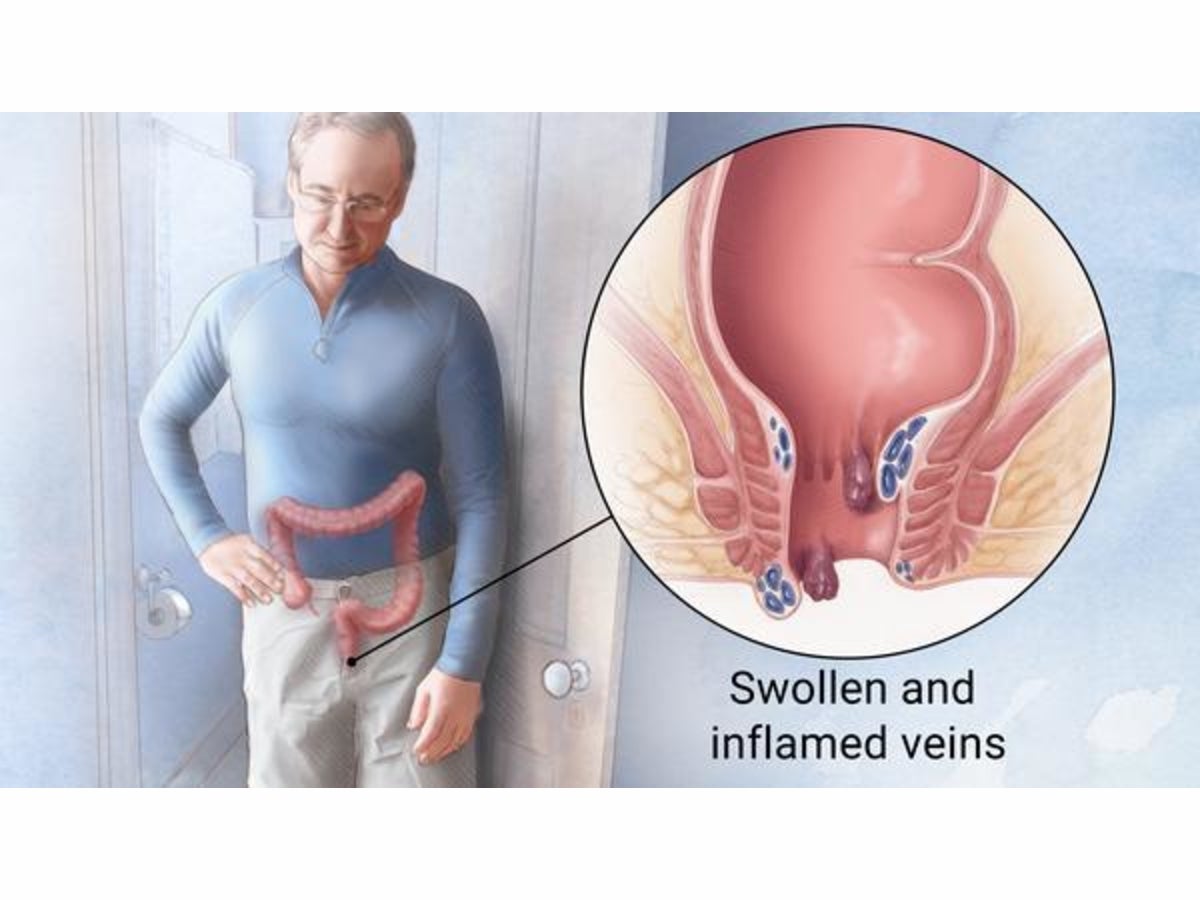
Haemorrhoid is called swelling or enlargement of the vessels in the last part of the large intestine, which we call anus or breech region. The veins in the anal canal tend to hang and sometimes squeeze. As time goes on, these tangles may come out of the breach.
Stages of Hemorrhoid;
1: Hemorrhoid is manifested by bleeding. Small bleedings may contaminate the toilet paper or sometimes in the form of drops. Haemorrhoid does not sag at this stage. However, it is seen by resectoscope.
2: Hemorrhoid hang out with defecation and then go back spontaneously.
3: Hemorrhoid nozzles are now out of the anus. They can only be pushed back into the anus by pushing with the finger. Very often, oedema occurs and causes pain.
4: The stage in which haemorrhoid hang out of the rectum. Nozzles are usually large and wet. Complaints include contamination of underwear due to inability to fully clean up after a large ablution, and pain may occur while sitting.
What are the Symptoms of Hemorrhoid?
Pay attention to these symptoms!
Common Haemorrhoid Symptoms;
- Pain or burning sensation during defecation
- Rectal bleeding (Fresh red bleeding from the rectum)
- Swelling, discharge or wetness in the breech
- Itching
- Irregularity in defecation
How is Hemorrhoid Diagnosed?
Many people are ashamed to see a doctor about haemorrhoid problems. Therefore, although 75% of the patients have a haemorrhoid, only 4% of these patients consult a doctor. A thorough medical examination will help your doctor recommend an effective treatment.
This also helps to exclude more serious causes for your symptoms. Your doctor can easily see if you have an external haemorrhoid. For internal haemorrhoid diagnosis, anal canal and rectum examination and other tests are performed.
The rectum examination is performed by the doctor by finger. It is decided whether further examination is required by examination. An internal haemorrhoid may not be detected by examination because they are too soft. Therefore, it may be necessary to examine the rectum and other parts of the large intestine with a device called a colonoscopy with a camera at the end. Your doctor may want to examine your entire large intestine using colonoscopy if:
- Signs and symptoms indicate that you may have another digestive system disorder
- If you have risk factors for large bowel cancer
- If you are middle-aged and have not recently undergone colonoscopy
How Does Hemorrhoid Treat?
The treatment is primarily aimed at regulating bowel movements. If you have problems such as constipation or diarrhoea that occurs continuously, the causes that cause it must be found and resolved first. Any haemorrhoid cream or medication should not be used until the definitive diagnosis of haemorrhoid is made by the attending physician. More like l.
and for the second stage, medication and cream treatment is applied. The cream is generally used to prevent pain, swelling and burning. Also, massaging the problem area with cream containing a small amount of nitroglycerin can reduce pain and burning. These creams can relax and relieve breech muscles. However, the creams used are creams with heavy effects. Do not take too much.
One of the methods of haemorrhoid treatment is to sit for 15 to twenty minutes with warm water in any tub after defecation. Disinfectant can be used in this method called sitting bath and provides relaxation. Then dry with breech paper towels.
Strangulation or band ligation is another treatment method developed. In this method, a rubber is attached around the haemorrhoid nozzle and the nozzle is allowed to rot. These are open and non-surgical treatment methods.
Anal Fissure (Breech Fracture)
What is Anal Fissure?
An anal fissure is a disease that causes severe pain and sometimes bleeding during and after defecation as a result of a cracked wound at the outlet of the breach. Although small in appearance, its discomfort is very evident. The crack occurs most in the rear midline.
Why Does Anal Fissure Occur?
It is known that long-term constipation, birth, inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis are effective in the formation and maintenance of fractures.
In most patients, a large and hard history of defecation before the onset of complaints or frequent bowel movements during diarrhoea is the event that triggered the disease.
The insertion of a rectal thermometer includes the tip of the enema device; even an endoscope used in the examination of the rectum and anus may cause a sufficient trauma to produce anal fissure.
What are the Symptoms of Anal Fissure?
The main complaint is a pain, which is exacerbated by bruising in the breech, a little lessened by pain and a few drops of bright red blood coming from the stool. Constipation may also accompany them.
- Pain in the breech
- Blood in stool
- Constipation
How is Anal Fissure Treated?
Constipation prevention is very important in the treatment of anal fissure. For this, plenty of fruit, vegetables should be consumed. Anal fissure in women is usually related to birth trauma or constipation in the first days after birth. If the anal fissure is formed, diet, faecal softening drugs, short-term topical creams, hot water sitting baths should be continued for up to 3 weeks, and if there is a pain, painkillers should be given.
The gold standard in surgical treatment is internal sphincterotomy, which is performed by local or general anaesthesia, and the internal muscle of the breach is cut and loosened. This method reduces the pressure in the region. After surgery, 97 to 100% of the fractures heal completely. More than 90% of patients relieve pain within 48 hours.
In addition, local ointments used in the treatment of anal fissure are effective by reducing the pressure in the anal canal, the rapid emergence of the positive effect of the drug, failure of the patient does not cause any harm and the side effects are extremely low, insignificant treatment methods have started to be preferred today.
Breech Abscess (Anorectal Abscess)
What is Anal Abscess?
An anal abscess occurs as a result of inflammation of the breach and pus collection. It usually arises from the inflammation of the breach glands and spreads. The main task of these glands is to facilitate faecal output by secreting mucus. It is an inflammatory disease that requires emergency surgery. Although it can be seen in every age group, it is more common between 30-40 years of age. Men also have a higher incidence than women. It is frequently seen in the spring-summer months when stool softness increases. It triggers the disease by blocking the perception of exit points of the aqueous stool glands.
What are the Symptoms of Anal Abscess?
It starts with pain in the breach region during defecation, and then symptoms such as redness, swelling and temperature increase. Patients also report fever, sweating, weakness and discharge from the rectum.
Why Does an Abscess Occur?
Surgical procedures applied to anal region, anal region trauma, presence of an anal fistula, previous history of anal abscess can be listed as risk factors for anal abscess formation. Sometimes it occurs after long-term diarrhoea. Excessive alcohol consumption and excess weight are among the risk factors.
How is Anal Abscess Spread?
Due to the pressure exerted by the increased amount of pus, the intersfincteric abscess spreads to the adjacent tissues surrounding itself, moving under the skin, reaching the perianal cavity and growing to form the perianal abscess. It runs upwards through the muscles and forms the supra levator abscess in the supra levator cavity. Or the sphincter muscle goes sideways and becomes an ischiorectal abscess.
How is the Diagnosis of Anal Abscess Diagnosed?
In most patients, the examination is sufficient for diagnosis. Sometimes ultrasound and MRI may be requested.
What are the Treatment Methods for Anal Abscess?
Anal abscess treatment aims to correct breech symptoms and general infection, as well as prevent the abscess from becoming complicated or triggering other pathologies such as anal fistula.
The treatment of an anal abscess is surgical. Abscess drainage is performed under anaesthesia, the closest location to the anus should be chosen for the incision. Once the abscess has been drained, pain, fever and other inflammatory symptoms will heal quickly. Antibiotics, painkillers and hot water sitting baths can be used in this healing process.
The patient is given antibiotic treatment after surgery and is followed up regularly. The recurrence rate is around 10%. Late admission of the patient with an abscess is important in terms of insufficient treatment of the abscess and the risk of fistula formation. Fistula formation occurs in 30% of patients with an anal abscess.
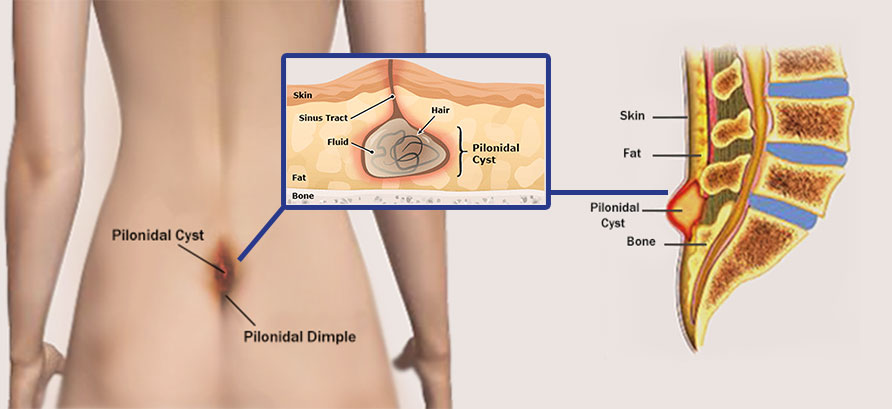
Bristle Rotation
Hair rotation is a skin condition that occurs mostly in men and the coccyx region. It occurs as a result of the hairs and hairs poured from the back, neck, scalp areas of the body into the skin from the pores or cavities and accumulate here to form a cystic structure. Inflammation may also occur in the area of hair rotation. In addition to the coccyx, it may also rarely be seen in other body parts such as navel.
What is Pilonidal Sinus?
In the medical literature, hair rotation, which is called “pilonidal sinus en, is a disease that can be prevented by providing hygiene conditions and removing hairs in the body at regular intervals. However, the only thing to do after the emergence of the disease is to apply to clinics and hospitals to get support from a general surgery specialist. Because hair rotation is not a discomfort that can pass spontaneously after a certain time.
Causes Hair Rotation (Pilonidal Sinus)?
Experts propose two different theories of the formation of the pilonidal sinus. The first of these is the accumulation of hairs and feathers shed from the body from the holes and pores under the skin, especially if there is sweating. It has been observed that the hairs entering the skin during the movement of the body can reach around 60 – 70.
The area where the bristles accumulate is surrounded by a membrane to form a cystic structure. The liquid produced as a reaction to the hair causes a malodorous abscess flowing out of the sinus mouth.
What Are the Symptoms of Pilonidal Sinus?
Symptoms that do not disturb the patient in the initial stage may become unbearable in later stages.
Some of the symptoms observed in almost all of the patients applying to the health facility due to hair turn are listed below;
- At the initial stage of hair rotation, the discharge problem occurs. Patients who meet this humidity in the underwear, as usual, are generally unaware of the case at this stage.
- This discharge, when combined with germs, turns into inflammation and turns green.
- The discharge is accompanied by a bad smell.
- Sometimes bloody discharge can also be seen.
- Other symptoms of hair rotation are itching, redness, swelling and pain in the rectum.
- Over time, the pain becomes so severe that the patient can no longer perform daily activities.
The reason for the bad smell seen in hair rotation is the inflammation and abscess of the related area. The currents coming out of the sinus mouth combine with the germs and prepare the ground for the formation of a foul-smelling and inflamed abscess.
The size of the swelling that occurs in the pilonidal sinus region varies according to the density of the hairs accumulated in the region. The pain caused by the stretching of the cyst into an abscess may have an unbearable severity.
The person may become unable to sit or walk due to this pain. The presence of a pain in which even everyday activities cannot be performed is a sign that the disease is in its final stage.
How is Hair Loss Treated?
The condition of the region is firstly considered in the treatment of hair rotation. Your doctor will apply the treatment you deem appropriate, depending on the situation in the region of hair loss.
- Preventive / Preventive Approach: If the condition is detected at an early level and there is no redness, swelling or pain in the coccyx, your doctor will control the immune system with broad-spectrum antibiotics to prevent the formation of cysts and abscesses.
- Surgical Intervention : Proctology is a sub-branch of general surgery and specializes in the diagnosis and treatment of breech diseases. Do not try to squeeze the cyst or abscess by yourself. This will cause you much pain, and this action, performed without the doctor’s control, makes the sensitized tissue vulnerable to other external diseases.
Although more than fifty surgical interventions have been developed over the years for the treatment of hair loss, only ten of them are currently in progress. Among these, Bascom is the most common type of surgery used in the treatment of hair rotation in the coccyx.
The main advantage of this method is that it enables the patient to continue his / her daily life without having to go to bed. The cyst or abscess is evacuated from the incision, which is about 2 centimetres in length, by identifying where the hair rotation occurs. The doctor may choose to close the incision or not, depending on the condition of the cyst.
Open Wound: In this preference, the doctor prefers not to close the wound and the hollowed area is healed from the inside to the outside and is completely closed. Although the healing time is longer in the choice of not closing the wound, the depression is completely closed, minimizing the risk of hair re-formation in the coccyx.
Stitched Wound: Although the healing time is much shorter in the choice of closing the incision with suture, the likelihood of relapse is very high. Some surgeons may prefer to accelerate the healing process by opting to cut the margins where healing is more difficult.
Anal Itching (Pruritus)
What is Pruritus?
Anal itching; It is a very common chronic problem that occurs in or around the anus. This pruritus can be caused by many reasons and may result from some diseases.
What are the Causes of Anal Itching?
- Parasitic diseases
- Hairworm,
- Leaving the breech area wet and moist after insulting
- Spicy foods, caffeinated drinks, milk and dairy products, tomatoes, nuts, nuts such as nuts to consume a lot,
- Wearing tight clothes and underwear to prevent air intake of the anus area,
- Irritation of urine and faecal residues due to insufficient hygiene, lack of hygiene
- As a result of excessive cleaning obsession around the anus by removing the protective secretion on the breech around the breech to make it more sensitive, more itching,
- Allergic reactions,
- Psychological causes (skin diseases caused by stress, anxiety, depression)
- In addition to all these reasons, itching may occur as a result of some diseases. These diseases include hemorrhoidal disease, anal fissure, Crohn’s disease.
Other Causes of Anal Itching:
- Warts around the breech,
- Skin cancer,
- Scabies,
- Fungal infection
- Psoriasis and eczema
- Parasitic worms are another cause of anal itching.
What are the Symptoms of Anal Itch?
The most common symptom occurs as a result of bowel movements Skin redness, discharge, skin irritation are the symptoms of itching.
Symptoms that require you to consult a doctor:
- Anal itching rash,
- If there are discharge, bleeding and especially fever,
- If there is hairworm, it is necessary to see a doctor.
What is the Diagnosis?
In addition to examination to diagnose, it is used to identify diseases that cause anal itching: various diagnostic methods such as anoscopy, rectoscope, sigmoidoscopy, colonoscopy, stool analysis, a skin biopsy or allergy testing.
Treatment Process
Firstly, it is investigated whether parasitic diseases that may cause anal itching cause itching.
At this stage:
various tests such as stool examination, blood tests, anoscopy, rarely colonoscopic evaluation, a skin biopsy can be performed.
Unless this type of disease-causing anal pruritus is detected, treatment methods are applied in many ways.
Among These Treatments;
- Personalized diets where some foods that cause itching are not consumed,
- Providing bathroom and necessary hygienic care
- Pomat application,
- Fungal treatment,
- There are applications such as methylene blue injection.
Steroid-containing / cortisone creams can be used for a very short time and zinc-oxide pomades can also be used.