Asthma
What is Asthma and Asthma Attack?
Asthma is a life-long (chronic = chronic) disease that requires long-term treatment.
In asthma, non-microbial inflammation (inflammatory) is seen in the airways.
What Are the Symptoms of Asthma?
In asthma, there is redness, swelling and narrowing of the airways in the lungs; this leads to recurrent respiratory complaints.
Excessive cough, wheezing, shortness of breath and chest pressure.
Symptoms of asthma worsening during exercise.
Symptoms of asthma caused by triggering factors such as dust, animal hair, pollen, cigarette smoke, changes in weather conditions or certain medications. Asthma attacks can range from slowly worsening attacks to rapidly worsening attacks.
How is Asthma Diagnosed?
For the diagnosis of asthma, first of all, the characteristics of the complaints and the presence of asthma in the family are questioned.
Shortness of breath, wheezing, coughing and pressure in the chest, especially during the night and/or morning.
Bouts of asthma caused by a warning such as allergens or cigarette smoke.
The presence of asthma and/or other allergic diseases in the family is important for the diagnosis of asthma.
Asthma complaints are not always typical as mentioned above. In this case, pulmonary function tests may be required.
Pulmonary function tests help to identify the presence and severity of airway stenosis as well as to distinguish some asthma-misdiagnosed diseases.
How to Treat Asthma?
Asthma may not be completely eliminated. However, asthma can be fully controlled by appropriate treatment and good patient-doctor collaboration.
Good control of asthma means fewer hospitalizations and improved quality of life.
Objectives of Asthma Treatment
For asthma patients, complaints are often the only goal. However, this expectation of patients may mask the actual situation. Because it is important to treat inflammation (inflammation).
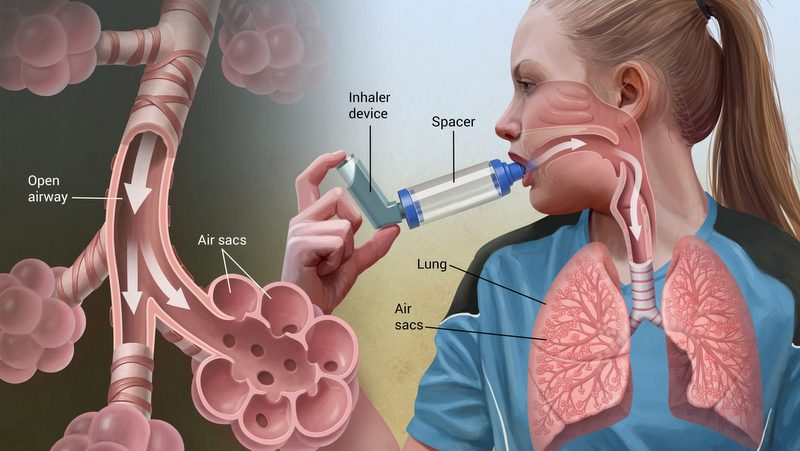
Two groups of drugs with different effects are used in the treatment of asthma:
- Controlling drugs
- Relaxing medicines
Most of the drugs used to treat asthma are given by inhalation; medicines thus reach the airways directly.
The goals of asthma treatment are:
- Lack of day and night complaints
- Making the work comfortable
- Little need for relaxing medication
- No need to apply to the emergency department
- Maintain control provided.
Controlling drugs
- Drugs in this group treat asthma and control asthma.
- Respiratory steroids belong to this group.
- These drugs should be used daily and for a long time.
- If the patient discontinues treatment without consulting his doctor, thinking that he has recovered, the disease will reappear.
Relaxing medicines:
- Effects are felt in a short time.
- This group of medicines should only be used to open the airways when there is a need for shortness of breath.
- If these drugs are heard, asthma does not heal.
Bronchiectasis (Bronchous Expansion)
What is Bronchiectasis?
Bronchiectasis is a condition in which the bronchial tubes in your lungs are permanently damaged, widened and thickened. These damaged air passages allow bacteria and mucus to accumulate in the lungs. This often results in infection and obstruction of the airways.
There is no treatment for bronchiectasis, but it is manageable. With treatment, you can live a normal life. However, exacerbations should be treated to ensure the flow of oxygen to the rest of your body and to prevent further lung damage.
Causes of Bronchiectasis?
Any lung injury can cause bronchiectasis. There are two main categories of this situation. One of these is associated with cystic fibrosis (CF) and is known as CF bronchiectasis. CF is a genetic condition that causes abnormal mucus production.
The other category is non-CF bronchiectasis not associated with CF. The most commonly known conditions that can lead to non-CF bronchiectasis are:
- An abnormal functioning immune system
- Inflammatory bowel disease
- Autoimmune diseases
- Chronic obstructive pulmonary disease (COPD)
- Alpha 1-antitrypsin deficiency (an inherited cause of COPD)
- HIV
- Allergic aspergillosis (an allergic lung reaction to fungi)
- Pulmonary infections such as whooping cough and tuberculosis
- CF affects other organs such as lungs, pancreas and liver. This can cause repeated infections in the lungs while disrupting the functioning of other organs.
Symptoms of Bronchiectasis
The symptoms of bronchiectasis may take months or even years to develop. Some typical symptoms are:
- Chronic daily cough
- Blood Spitting
- Wheezing or breathing through the chest
- Shortness of breath
- Chest Pain
- Removing large amounts of phlegm
- Weight Loss
- Fatigue
- Bad breath
- Frequent respiratory infections
- Developmental retardation in children
- If you experience any of these symptoms, you should consult your doctor immediately for diagnosis and treatment.
Treatment of Bronchiectasis
There is no cure for bronchiectasis, but treatment is important to help you control the condition. If it is discovered early and infections are kept to a minimum, the damage may slow down and the condition may be easier to manage.
It is also critical to prevent further blockage of the airways and to minimize lung damage. Common methods for the treatment of bronchiectasis include:
- Airway cleaning methods (such as breathing exercises and chest physiotherapy)
- Pulmonary rehabilitation
- Antibiotics to prevent and treat the infection
- Bronchodilators such as albuterol (Proventil) and tiotropium (Spiriva) to open the airways
- Sputum Thinner
- Oxygen therapy
- Vaccines to prevent respiratory infections
If there is bleeding in the lung or bronchiectasis is only part of your lung, surgery may be necessary to remove the affected area.
If conditions such as immune disorders or COPD cause bronchiectasis, treatment of these diseases is necessary.
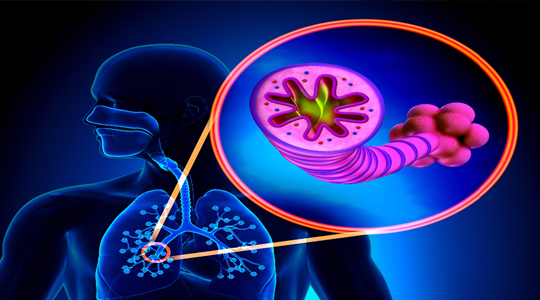
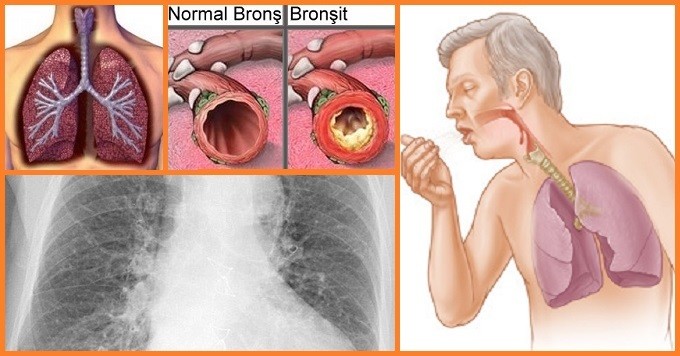
Bronchitis
What is Bronchitis?
Inflammation caused by infection of small air sacs, called bronchioles, causes constriction of the sacs, resulting in greatly reduced lung capacity. Acute bronchitis is the most common condition of the lower respiratory tract.
What are the Symptoms of Bronchitis?
Acute bronchitis usually occurs following upper respiratory tract infection, and the first symptoms observed in the presence of the disease are usually signs of upper respiratory tract infection such as sneezing and runny nose.
Increased infection in the bronchioles may cause high fever and loss of appetite.
As the disease progresses, respiratory distress is observed with the filling of the air sacs and the congestion rate increases.
Increased respiratory distress causes the patient to experience sudden transient cough crises.
One of the most prominent clinical manifestations of the disease is wheezing.
Diagnosis of Bronchitis
The clinical picture of acute bronchitis and asthma bronchitis is very similar and may lead to confusion. Particularly during the first episode of bronchitis, this distinction is extremely difficult to make, but the diagnosis becomes easier with the clinical findings that occur during ongoing attacks. In this respect, the absence of signs of viral infection before bronchitis attack, frequent recurrence of wheezing episodes, presence of a family history of atopy or asthma is strong signs that support the disease as bronchitis asthma.
After the diagnosis of bronchitis, clinical grading is performed to determine the severity of the disease. When performing this procedure, the patient’s respiratory rate, wheezing, retraction and disturbances in the general condition (restlessness, loss of appetite, unconsciousness, etc.) are taken into consideration.
How is Bronchitis Treatment Done?
The goal in treating acute bronchitis is to apply supportive care to the patient and minimize discomfort by reducing symptoms. Treatment is started with bronchodilator (which leads to an expansion in the bronchi) agents in order to normalize the oxygen percentage in the patient and to relieve respiratory distress.
In patients who do not respond to bronchodilator treatment, who have recurrent respiratory attacks and who have severe bronchitis, the anti-inflammatory effect of corticosteroids may be utilized. The effectiveness of the drug therapy applied to the patient should be evaluated at regular intervals, so the whole treatment should be planned by the specialist doctor.
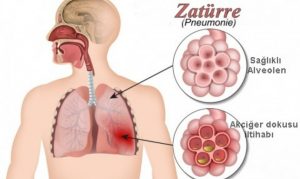
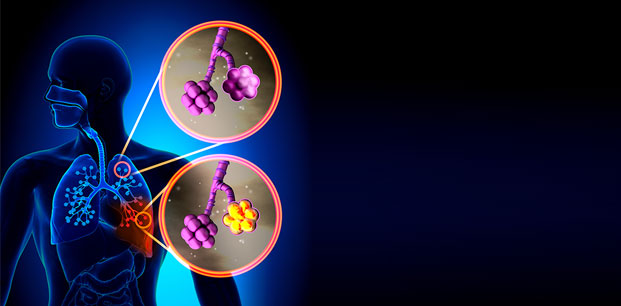
Pneumonia
What is Pneumonia?
Pneumonia is commonly known as pneumonia; briefly inflammation of the lung tissue. It occurs due to various microorganisms, especially bacteria. In some types of pneumonia, there is a direct risk of transmission from a sick person to healthy persons. However, the disease usually occurs when microbes in the patient’s own mouth, throat or digestive tract reach the lung. These microbes, which do not normally cause disease, produce pneumonia in people with weakened body defences. Therefore, rather than contamination, the risk factors that break the person’s body resistance play a role in the development of pneumonia.
What are the Symptoms of Pneumonia?
There may be chills, tremors, high fever up to 39-40 ° C, cough, dirty, inflamed (green, yellow, rust) sputum and side pain. Some types of pneumonia are insidious onset. Symptoms such as dry cough, fever, nausea, vomiting, a headache may occur following a few days of loss of appetite, weakness, joint and muscle pain.
Patients with this complaint should consult a doctor. Pneumonia is a health problem that should not be neglected. Early diagnosis and delayed treatment are known to reduce mortality. If the patient’s complaints are compatible with pneumonia, diagnosis can usually be made by examination and chest X-ray findings. Blood and sputum tests can be performed if necessary.
Is Pneumonia Contagious?
Influenza and similar viral respiratory infections that predispose to pneumonia are highly contagious. They can be spread by sneezing and coughing and can be passed on to other people through items such as glasses, handkerchiefs, forks and spoons contaminated with mouth and nose secretions. Pneumonia is one of the most common and most fatal diseases in the world and in our country. Pneumonia can be more fatal, especially in infants, children, the elderly and people with other known diseases. There are several risk factors that make it easier for a person to develop pneumonia. If it is possible to prevent them, pneumonia can be prevented.
Risk factors that facilitate the development of pneumonia in adults:
Advanced age:
Chronic diseases: Lung diseases (COPD, bronchiectasis, lung cancer), heart diseases, kidney diseases, liver diseases, diabetes, nervous system diseases (muscle diseases, strokes, dementia), swallowing difficulties (jaw, muscle, nerve diseases, tumors, esophageal diseases), immune system diseases (AIDS, blood and lymph gland cancers)
- Smoking
- Alcohol intake
- vomiting
- Previous long-term operations
- Flu Outbreaks
What are Ways to Prevent Pneumonia?
In order to prevent pneumonia, negative factors that facilitate the formation of pneumonia should be corrected. For this purpose, proper follow-up and treatment of chronic diseases, stress avoidance, balanced nutrition and hygienic shelter conditions should be ensured, alcohol, tobacco and drug dependence control should be reduced and the risk factors leading to aspiration of mouth and stomach contents into respiratory tracts should be reduced.
During influenza outbreaks that can lead to or facilitate pneumonia, reducing contact in the crowd, wearing masks and vaccination of people who can infect influenza into the high-risk group are important for protection.
Continue
The influenza virus itself can lead to pneumonia as well as to facilitate the emergence of pneumonia from other microorganisms. Flu cases are severe and fatal, mostly pneumonia is associated with the flu. Therefore, influenza outbreaks must be prevented in order to prevent pneumonia and related deaths.
Vaccines have been developed to prevent influenza. These vaccines provide protection for one year. Influenza vaccines should be administered intramuscularly every year in September, October or at the latest in November. Influenza vaccines should be administered to people at high risk of influenza or to those with severe influenza if the flu is severe.
Pneumonia Treatment
In many cases, pneumonia can be treated at home. Severe cases, elderly patients, patients requiring oxygen therapy or intensive care support should be admitted to hospital. Treatment varies according to the patient. The results are promising when the treatment is started early and can be treated as an outpatient. However, the mortality rate is high in severe pneumonia cases with delayed diagnosis and treatment.
What is Tuberculosis?
Tuberculosis, or more commonly known as tuberculosis, is a disease that affects the lungs and renders them unable to function. It is a preventable and curable disease under the right conditions.
Its germ, after entering the body for a long time without the disease can stop. In this case, the body defends against the tuberculosis germ and imprisoned it. This condition is called tuberculosis infection. And it is only when the skin test is performed with the tuberculin test that the person facing such a condition is infected.
Causes Tuberculosis?
Tuberculosis is caused by a bacterium called “mycobacterium tuberculosis”. There are different varieties of this disease, and some may develop drug resistance. Tuberculosis bacteria are transported in airborne droplets. From the moment it enters the air, another human can breathe these bacteria. To answer the question of how tuberculosis is transmitted;
- Sneeze
- Cough
- Talk
- Singing
It can be infected with the road. People with strong immune systems may not have symptoms of the disease, even if they are carriers of bacteria. This is called a potential or inactive infection. According to the World Health Organization report, a quarter of the world population is a carrier of tuberculosis bacteria. Bacteria seen in inactive carriers are not contagious but can become active over time and make both the carrier and the surrounding people sick. Bacteria seen in inactive carriers are not contagious but can become active over time and make both the carrier and the surrounding people sick.
What are the Symptoms of Tuberculosis?
In a case called latent tuberculosis, bacterial carriers do not show signs of the disease. In these cases, the bacteria causing tuberculosis are dormant and it may take years for them to wake up and make them sick. Active tuberculosis is characterized by respiratory system disorders such as bloody cough and sputum. In the case of tuberculosis, the patient may experience painful coughing attacks that last three weeks and make it difficult to breathe normally. However;
- Fatigue without reason
- Fire
- Night sweating
- Loss of appetite
- Symptoms such as weight loss may also indicate tuberculosis.
Although tuberculosis commonly affects the lungs, it can also affect other organs of the body, such as the kidneys, spine, bone marrow, and brain. Symptoms vary depending on the organ affected by the bacteria.
How is Tuberculosis Diagnosed?
The symptoms alone are not sufficient for the patient to be tested for tuberculosis because they can be seen in many diseases. Since different tests may be performed on the discretion of the doctor, the answer to the question of how to perform the tuberculosis test varies according to the type of test.
 1.Tuberculin skin test
1.Tuberculin skin test
This test, which is generally used in Tuberculosis Dispensary, is the most common method used to determine whether a person has tuberculosis. In this test, the patient is injected with 0.1 millilitres of PPD just below the skin. The results will be announced in two to three days. If a 5-millimetre line is formed at the site of injection, the test result is considered positive. However, this test only detects whether the person is affected by the bacteria, but does not provide any results as to whether the bacteria are active or asleep.
2.Blood test
If the desired result is not obtained from the skin test, a blood test is performed. This blood test is also preferred to detect other infections that are unlikely to occur in the skin test. The results of the blood test may be positive, negative or uncertain. However, it is not possible to determine whether the bacteria are active or not in the blood test as in the skin test.
3.Chest X-ray
If your skin and blood tests are positive, your doctor will ask you to have a chest X-ray. In this X-ray, small but prominent spots in the lungs are sought. These points are indicative of tuberculosis infection and indicate whether the immune system is able to isolate bacteria. If the result of your chest film is negative, it is concluded that you are latent tuberculosis. However, if the dots are not visible, the result of all your tests may be inaccurate and must be done all over again. Unlike other tests, the X-ray shows whether the bacteria are asleep or active.
4.Other tests
Depending on the results of your other tests, your doctor may require a sputum or mucus test. These substances are taken from your lungs and used for the detection of tuberculosis bacteria. If the result of the sputum test is positive, active tuberculosis bacteria are mentioned and the patient is asked to wear a mask to prevent transmission. It is important both for the patient and his surroundings that the patient does not remove the mask until his results become negative. In order to detect tuberculosis,
- Computed tomography
- Bronchoscopy
- Lung biopsy methods can be applied.
How is Tuberculosis Treated?
As with other bacterial infectious diseases, a few weeks of antibiotic treatment is not sufficient in tuberculosis. Active tuberculosis patients have to take many different drugs for 6 to 9 months. Drug treatment and routine controls should not be interrupted until the test results return to negative, otherwise, the infection will relapse.
If the disease reoccurs even though treatment and controls are not interrupted, the bacteria may have acquired resistance to the drugs and need to be replaced. Since the TB germ is resistant to the active substance of many drugs, many different drugs should be taken together.
Patients receiving tuberculosis treatment should pay attention to the main symptoms of liver disease. These symptoms include:
- Anorexia
- Darkness in urine
- Fever lasting more than three days
- Nausea and vomiting for no reason
- Jaundice or yellowing of the skin
- They manifest themselves in the form of abdominal pain.
Continue
If you are receiving tuberculosis treatment and one or more of these symptoms occur, you should see your doctor immediately. In order to prevent these symptoms, you should also check your liver for proper functioning with a regular blood test.
In addition to drug treatment, nutrition is very important in the treatment of tuberculosis. By maintaining a healthy diet for the patient, it is important for him to maintain his ideal weight, or if he is overweight, to maintain body resistance. In addition, reducing the consumption of refined flour and sugar, avoiding alcohol and taking foods rich in minerals makes it easier to get over the disease.
Pulmonary Hypertension
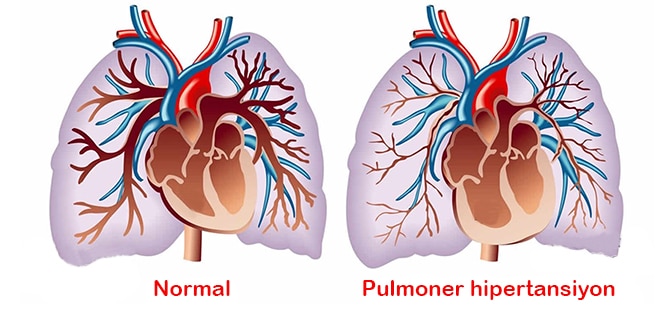
What is Pulmonary Hypertension?
It is located on the right side of the heart and is poor to the lung; that is, the pulmonary artery that is responsible for delivering contaminated blood to oxygenate it is called the pulmonary artery. Pulmonary hypertension, on the other hand, refers to the continuous high blood pressure associated with the lung. Pulmonary hypertension, defined as high blood pressure in the pulmonary artery, was described in 1891 by Dr Ernst von Romberg. Pulmonary hypertension, which is in the class of serious and dangerous diseases, must be kept under the supervision of a doctor and treatment should be started as soon as possible.
Pulmonary hypertension, which directly affects the heart, can lead to heart failure in later stages if precautions are not taken.
What is the Occurrence of Pulmonary Hypertension?
The so-called pulmonary artery is the pulmonary artery responsible for delivering contaminated blood from the right ventricle of the heart to the lungs. Clogging or narrowing of the thin branches and capillaries of the pulmonary artery results in significant resistance to blood flow.
As a result of this resistance, the right ventricular, which pumps blood more intensely, is constantly exposed to high resistance and expands over time, causing heart failure. Although the cause of pulmonary hypertension is not yet known, it may occur as a result of damage to the cell structure in the pulmonary arteries or loss of some important functions.
What Causes Pulmonary Hypertension?
The cause of pulmonary hypertension is not yet known. However, in the disease, which is thought to play an effective role, various factors, from the drugs used to the various lung diseases, trigger the disease. Pulmonary hypertension, which is thought to be effective in genetic factors, plays a role in many factors ranging from dietary drugs to heart failure.
To list the diseases that cause pulmonary hypertension;
- Aortic and mitral valve diseases
- Heart failure
- Congenital heart diseases
- Chronic liver disease
- COPD and lung diseases
- Lung tumour
- Pulmonary fibrosis
- Emphysema
- Cirrhosis
- Rheumatic diseases
- Scleroderma and SLE (lupus)
Symptoms of Pulmonary Hypertension
Symptoms may vary from patient to patient, and generally, no symptoms are observed in the early stages of the disease. Shortness of breath is the main symptom of pulmonary hypertension. Shortness of breath In the early stages of the disease, shortness of breath after exerting efforts such as climbing stairs and exercise is also observed later on at rest.
Let us briefly list the symptoms of pulmonary hypertension;
- Dizziness
- Fatigue
- Feeling powerless
- Shortness of breath
- Chest Pain
- Squeezing in the chest
- Palpitation
- Cough
- Skin and lips turn bluish
- Oedema of the ankles
- Liver growth
- Abdominal swelling
Diagnosis of Pulmonary Hypertension
Pulmonary hypertension, which is usually diagnosed in the late stages of the disease, shows the same symptoms as many diseases. Therefore, it is one of the most difficult diseases to diagnose. As in all diseases, early diagnosis is very important in pulmonary hypertension. Because pulmonary hypertension shows the same symptoms as many diseases, a very detailed examination is required. As a result of the detailed investigations and examinations, the correct diagnosis should be made and treatment should be started as soon as possible.
Examinations for Diagnosis of Pulmonary Hypertension
- Blood analysis
- ECG
- echocardiography
- Transesophageal echocardiography
- Lung tomography
- Pulmonary function test
- Lung ventilation-perfusion scintigraphy
- 6-minute walk test
- Heart Catheter
- Pulmonary arteriography
Pulmonary Hypertension Treatment
There is no definitive treatment for pulmonary hypertension. However, with the treatments applied, it is aimed to minimize the complaints of the patient and to prevent the progression of the disease. In the case of a disease that is effective in the development of pulmonary hypertension, treatment of this disease is carried out first.
It is very important that the patient protects himself against respiratory infection. Therefore, it is recommended that patients with pulmonary hypertension stay away from people suffering from respiratory tract infection. Drugs used in the treatment process are aimed at preventing problems such as blood clotting and heart contractions. However, if the patient does not respond to all these medications and his condition worsens, heart or lung transplantation is the last resort.
Cystıc Fıbrosıs
What is it?
Cystic fibrosis (CF) is a genetic disease that is caused by the transmission of defective genes from the mother and father to the child. It is not contamination or subsequent illness.
Since the symptoms are similar to the common disorders in childhood, the patient may be delayed in diagnosis. If the course of the disease is not done well, mild symptoms may be replaced by organ involvement and may even result in death. Although lung involvement is an important factor determining the prognosis of the disease, malabsorption due to pancreatic involvement is also one of the factors affecting survival.
What Causes Cystic Fibrosis?
It is a genetic disease. In other words, the most common cause of the disease is the mutation of the gene from both parents.
Symptoms:
- Although it varies according to the affected organ, it may present with many findings.
- In early infancy, recurrent and treatment-resistant lower respiratory tract infections, cough, wheezing may occur.
- Patients may have difficulty in gaining weight, oily, smelly and frequent defecation, growth and developmental retardation.
- When they are kissed by their mother, it may be felt that they have excessive salty sweat.
- They may apply with loss of liquid and salt, weakness, loss of appetite and exhaustion, especially in hot weather.
- In older children, symptoms may include excessive sputum production, frequent lung infection, enlargement of the fingertips (clubbing), nasal polyps, recurrent attacks of sinusitis.
- Rarely, it may present with findings such as diabetes.
- Adulthood, delayed puberty, pancreatitis attacks, hepatic and pancreatic insufficiency can be seen in adulthood.
How is Cystic Fibrosis Diagnosed?
Complaints such as symptoms of cystic fibrosis can also be varied. Anaemia, elevation in liver function tests, impaired chlorine values and changes in blood gas, pulmonary as well as chest film findings are among the methods used for diagnosis of cystic fibrosis. The exact diagnosis is made by the presence of chlorine elevation in the sweat test. Values taken as a result of this test of 60 and above mean cystic fibrosis. At the same time, the cystic fibrosis gene mutation analysis structures can be determined by the type of mutation in which the disease occurs.
How is Cystic Fibrosis Treated?
Cystic fibrosis is treated with a combination of medication, physical therapy and exercise.
Drug: There are three main drugs used in the treatment of Cystic Fibrosis.
Bronchodilator drugs that keep the airway open, antibiotics fighting infections, steroids to alleviate inflammation. To help digestion, patients with Cystic Fibrosis need to take pancreatic enzymes with each meal.
Physiotherapy: Daily physical therapy is inevitable for clearing the mucus layer in the airways and minimizing infection. This physiotherapy can be administered by the parent or caregiver at home. When children are old enough, they can apply the necessary daily therapies themselves. Exercise Daily exercises are an important part of the treatment and management of Cystic Fibrosis.
Bronchopulmonary Dysplasia (BPD)
In premature babies, babies have problems in breathing due to lungs that have not completed their development. Most of these babies breathe in the first days with the help of breathing apparatus (ventilator), they may need to take oxygen therapy for a long time. Injuries and inflammation of premature lung tissue and airways that may not develop during these treatments may develop.
A premature baby is diagnosed with bronchopulmonary dysplasia (BPD) or chronic lung disease if it requires oxygen therapy when it is 28 days old. These babies need additional oxygen and sometimes breathing aid.
Symptoms
Infants with bronchopulmonary dysplasia are struggling to breathe and show signs of distress along with other respiratory problems. These signs;
Fast, superficial breathing, Pulls in ribs and chest wall, Cough, Movement of chest wall and abdomen in opposite directions at each breathing, Wheezing (a whistling sound when baby breathing), Stance on the neck, shoulders and upper body, Repetitive bruising periods Apnea respiratory arrest)
Diagnosis
Diagnosis is often made when a premature baby with respiratory problems requires additional oxygen supply for more than 28 days. It can only be said that a baby is BPD after weeks of birth. Infants with BPD often have spongy images filled with blisters on lung films.
Treatment
There is no special treatment and usually, supportive treatment is given. Supportive treatment includes providing the baby with adequate oxygen, regular feeding, keeping warm, protecting or treating infections, and administering appropriate amounts of fluid and nutrients. This saves time for the baby to develop into the lungs. Babies with BPD usually receive treatment in neonatal intensive care units.
The most important treatment of BPD is to prevent the formation. Prevention efforts can be listed as follows:
Prevention of preterm labour: Regular prenatal care will reduce the number of preterm babies in women at high risk of preterm labour. Steroid treatment will help maternal lungs to mature.
External surfactant administration: Surfactant is a fluid that normally covers the inner surface of healthy, developed lungs. The surfactant allows easy opening of the lungs and prevents them from completely closing. A lung that breathes normally gets more oxygen.
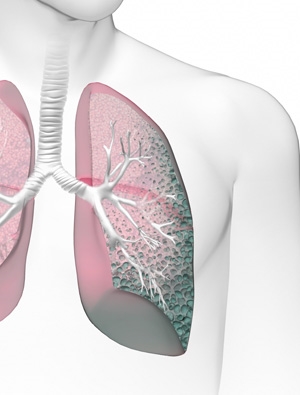
Pulmonary Embolism
What is Pulmonary Embolism?
Pulmonary embolism is a health problem caused by a blocked blood vessel in the lungs. In the medical literature, the condition called pulmonary embolism can cause life-threatening consequences if not treated quickly. This blockage of the pulmonary arteries can damage the lungs and other organs that cannot get enough oxygen. It is a serious condition and may take weeks or months of recovery.
Causes Pulmonary Embolism?
Pulmonary embolism occurs when a material with a blood clot often reaches an artery in the lungs causing obstruction. These blood clots most often come from deep veins in the legs. This condition is known as deep vein thrombosis (DVT). Occasionally, blockages in the blood vessels can be caused by substances other than blood clots. Some of these materials;
- Fat, collagen or other tissue from a broken, long bone marrow
- Part of a tumour
- Can be sorted in the form of air bubbles.
What are The Risk Factors for Pulmonary Embolism?
Although everyone may have a blood clot resulting in pulmonary embolism, some factors cause an increased risk. Risk factors for pulmonary embolism are described in detail below.
Patient’s Medical History
History of a venous blood clot or lung embolism in the past poses a high risk for a new embolism. In addition, certain medical conditions and treatments seen in the patient cause an increased risk of embolism. Some of these factors are;
- Cardiovascular diseases. Cardiovascular diseases
- Pancreatic, ovarian and lung cancers and many types of cancer spread to distant parts of the body increase the levels of certain substances involved in blood clotting, increasing the risk of lung embolism.
- Surgical procedures are one of the leading causes of blood clotting. Before and after major surgical procedures, the patient may be given anticoagulant medications.
Long Inactivity
Blood clots are more likely to occur during periods of prolonged immobility, such as:
- Rest cure. Postoperative, long-term bed rest due to heart attack, leg fracture, trauma or any serious illness makes the person more vulnerable to blood clot formation.
- Long journeys. Sitting in a cramped position during prolonged aeroplane or car travel slows blood flow in the legs and examines clot formation.
Other Risk Factors
- Being overweight. Obesity,
- Get estrogen support.
- The baby’s compression of the vessels around the uterus can slow the return of blood from the legs.
What are the Symptoms of Lung Embolism?
Symptoms of pulmonary embolism; the extent to which the lungs are affected, the size of the clots, and the presence of underlying lung or heart disease.
- Shortness of breath. Characteristically, it appears suddenly and tends to deteriorate with effort.
- Chest pain. It may increase when deep breathing, coughing, eating, bending or resting.
- Bloody and sputum cough can be seen.
- Pain in the back
- Excessive sweating
- Dizziness
- Fainting
- Blue lips and nails
Other symptoms that may occur with pulmonary embolism may include;
- Leg pain or swelling that usually occurs in the calf
- Moist and pale skin (cyanosis)
- Increase in body temperature
- Excessive sweating
- Fast or irregular heartbeat
- Feeling dizziness or evil
In addition to the symptoms listed, pain, redness and swelling may occur on one of your legs (usually the calf).
How is Lung Embolism Treatment?
If lung embolism is suspected to be an emergency, the patient is given an anticoagulant injection before the desired test results are obtained for a definitive diagnosis. These drugs, called anticoagulants, prevent the growth of existing blood clots and the formation of new clots. If the tests confirm the presence of pulmonary embolism, anticoagulant drug injections are continued for at least 5 days. In addition, oral anticoagulant tablets are given for the following 3 months. Full recovery is expected with early diagnosis and treatment. Rarely, surgery may be needed to remove the clot from the lung.
How Long Does Lung Embolism Treatments Last?
In pulmonary embolism due to deep vein thrombosis, treatment with blood thinners is continued for 3 to 6 months. Patients with prior blood clots should use medication for longer periods of time. If there are risk factors such as cancer treatment, treatment is continued as long as the risk factors continue.
Related
Lung Cancer
What is Lung Cancer?
Lung cancer, where smoking is one of the main factors, ranks first in cancer-related deaths. However, when caught at an early stage, the chance of treating the disease increases.
Lung cancer begins when cells from structurally normal lung tissue proliferate beyond the need and control to form a mass (tumour) within the lung. The mass formed here grows primarily in its environment, and in later stages, it spreads to the surrounding tissues or to the distant organs (liver, bone, brain, etc.) through circulation and causes damage.
Symptoms
- Increasing Cough
Cough, which is among the first symptoms of lung cancer, is often underestimated due to other reasons. However, persistent cough, which lasts more than two weeks, is increasing and the cause of which cannot be determined is the main indicator of lung cancer. However, the presence of sputum blood or the colour of sputum is dark brown is also known as important symptoms of lung cancer.
- Chest Pain
Again, chest pain, which can be caused by many reasons, is actually one of the main symptoms of lung cancer. Chest pain deep breathing, coughing or laughing increases if you need to consult a doctor immediately.
-
Shortness of breath
Respiratory symptoms such as shortness of breath and wheezing may occur in all stages of lung cancer. Shortness of breath, which is an important indicator of insidious lung cancer, is ignored properly.
- Anorexia and Weight Loss
Especially active smokers should consult a physician if they have anorexia. Unidentified cause of weight loss is among the important symptoms of lung cancer, should not be neglected.
-
Hoarseness and Swallowing Difficulty
One of the symptoms of lung cancer, hoarseness and difficulty swallowing can be caused by many reasons just like other symptoms.
- Fatigue
Rapid fatigue, constant fatigue and weakness in lung cancer are also common symptoms that should not be missed.
-
Pinning of Fingers
The slow and painless development of clubbing caused by swelling and rounding of the soft tissue at the tips of the fingers and toes shows that it is due to non-lung cancer reasons. However, the rapid and painful occurrence is among the symptoms of lung cancer.
-
Body Pain
In our country, especially complaints of back and shoulder pain are common, while desk employees can often consider this as a problem caused by poor posture and long hours working at a computer. However, in the case of lung cancer spread back pain, shoulder pain, shoulder blade pain, arm, leg pain, or severe headache if it has spread to the brain manifests itself as important symptoms. The growth in the glands on the neck and on the collarbone indicates lung cancer in particular.
- Frequent Recurrent Infection
Frequent recurrence and non-healing of respiratory infections such as bronchitis and pneumonia are among the symptoms of lung cancer.
-
Falling Eyelid
The fall of the eyelid and the reduction of the pupil and sweating on the same side of the face can also indicate lung cancer. This is called Horner syndrome in medicine.
Diagnostic Methods
Many methods are used for diagnosis. Since this cancer rarely presents symptoms before spreading to nearby lymph nodes or other organs, only 15 per cent of patients can be diagnosed early. Early diagnosis, often incidentally, occurs during examinations of another disease.
Today, some methods used in the diagnosis of lung cancer are as follows:
- Radiological examinations (Chest X-ray, Computed Tomography, Magnetic Resonance Imaging, PET / CT) in addition to sputum sample examination,
- Endoscopic evaluation of bronchi (bronchoscopy),
- Bronchoscopic or chest wall biopsy,
- Mediastinoscopy and video-assisted thoracoscopic surgery for the evaluation of mediastinal lymph nodes.
Treatment Methods
The most important factors in determining the treatment of lung cancer type and stage of cancer. Inappropriate patients, lung or lung section with cancer can be removed by surgical methods. Chemotherapy can be applied to patients who are considered unsuitable for surgery.
In addition, new treatments such as smart drugs and immunotherapy can also be used if cancer cells have specific properties.
Prevention of Lung Cancer
- Avoiding cancer-causing substances such as smoking and alcohol,
- Think positive and avoid stress,
- Avoiding radiation,
- Tar, gasoline, dyes, asbestos and so on. to ensure that substances are not inhaled,
- Avoiding air pollution,
- Maintain healthy eating scheme.
Lung Hardening (Idiopathic Pulmonary Fibrosis (IPF))
What is Lung Hardening?
The disease, abbreviated as IPF, causes the lung structure to become stiff and causes problems in breathing. The disease progresses very quickly in some patients and progresses slowly in some patients. The most important condition of the disease is that it may cause respiratory failure.
What are the Findings of Lung Hardening?
The first stage findings of Lung Stiffness are listed below.
- Stubborn cough without sputum,
- Shortness of breath even during daily activities,
- However, as the disease reaches advanced levels, the symptoms become more prominent.
The symptoms observed in this case are as follows.
- Difficulty breathing even when resting,
- The existing dry cough becomes more severe and turns into cough crises,
- Fatigue and strain even in easily performed activities,
- Clubbing or clubbing
- Fainting and drowsiness due to a decrease in oxygen saturation present in the blood.
These symptoms are observed in advanced levels of IPF. It must be treated.
How is the diagnosis diagnosed?
The definitive diagnosis of the disease is made by a surgical sampling of lung tissue. However, in cases where there is a typical image for IPF on lung tomography and there is no other disease to cause, it can be diagnosed without surgery. The severity of the disease is assessed by the appearance on lung tomography, pulmonary function tests and exercise tests. During the course of the disease, complaints increase and lung capacity and functions decrease.
How is it treated?
For many years, the search for an effective treatment for IPF has been continuing. Although various drugs have been tried as a result of the studies, there is no method to stop or treat the progression of the disease. The only definitive treatment is lung transplantation. Since there is no effective treatment, it is recommended that the patient be evaluated for lung transplantation as soon as the disease is diagnosed.
However, there have been promising developments in recent years. It has been observed that the progression of the disease can be reduced with new drugs which are being used in patients with IPF. However, it is seen that this effect can be achieved if treatment is started in the early stages of the disease.
COPD (Chronic Obstructive Pulmonary Disease)
What is COPD?
COPD, which is named with the initials of Chronic Obstructive Pulmonary Disease, is the result of obstruction of air sacs in the lungs called bronchus; It is a chronic disease that causes complaints such as dyspnea, cough and shortness of breath.
With breathing, the fresh air that is filled into the lungs is absorbed by the bronchi and the oxygen in the fresh air is delivered to the tissues with blood. When COPD occurs, the bronchi are blocked and cause a significant decrease in lung capacity. In this case, the fresh air taken from the lungs cannot be absorbed sufficiently, so that adequate oxygen delivery to the blood and tissues cannot be achieved.
How is COPD Diagnosed?
If the person smokes, the presence of long-term dyspnea, cough and sputum complaints is considered sufficient for the diagnosis of COPD, but a respiratory test should be performed for a definitive diagnosis. The respiratory assessment test, which is performed in a few minutes, is performed by deep breathing and blowing into the person’s breathing apparatus. This test, which provides easy information about lung capacity and the stage of the disease, if any, should be done at least once a year, especially for people over 40 years of age.
What Are the Symptoms of COPD?
“What is COPD?” Another point that is as important as the answer to the question of COPD symptoms and symptoms are considered to be followed correctly. As lung capacity decreases to a great extent due to the disease, sufficient oxygen delivery to the tissues cannot be achieved, and symptoms such as cough and sputum are observed, especially shortness of breath.
The problem of shortness of breath as a result of activities such as rapid walking, climbing stairs or running during the initial stage becomes a problem that can be observed even during sleep in the later stages of the disease.
Although cough and sputum problems are seen only in the early stages of the morning, symptoms of COPD such as severe cough and intense sputum are observed with the progression of the disease.
What Causes COPD?
It is known that the biggest risk factor for the occurrence of COPD is the consumption of cigarettes and similar tobacco products and the incidence of the disease is increased in people exposed to the smoke. Research conducted by the World Health Organization, COPD disease in the emergence of polluted weather conditions have shown to be largely effective.
At workplaces; It is observed that air pollution caused by dust, smoke and chemicals and organic fuels such as wood and dung used in domestic environments cause blockages in the bronchi and lung capacity is greatly reduced.
What are the stages of COPD?
According to the severity of the symptoms, the disease is named in four different stages: mild, moderate, severe and very severe COPD.
Mild COPD: Symptoms of shortness of breath, which may occur during intense work or during activities that require effort, such as climbing stairs or carrying loads. This stage is also known as the initial stage of the disease.
Moderate COPD: A stage of COPD that does not interrupt night’s sleep but causes shortness of breath during simple daily tasks.
Severe COPD: It is the stage of the disease in which the complaint of shortness of breath interrupts even the night’s sleep, and the weakness problem due to respiratory distress prevents daily work.
Very Severe COPD: In this stage, breathing becomes extremely difficult, the person has difficulty walking even in the home and the tissues do not transmit enough oxygen to various organs due to discomfort. Due to progressive lung disease, heart failure may develop and the patient cannot survive without oxygen supplementation.
What are COPD Treatment Methods?
Treatment of COPD usually involves attempts to reduce the severity of symptoms and disorders, not to eliminate the disease. The first step for treatment at this point should be to quit smoking, if used, and to move away from air pollution environments. With the cessation of smoking, the severity of congestion in the bronchi is alleviated to some extent and the person’s complaints of shortness of breath are greatly reduced.



 1.Tuberculin skin test
1.Tuberculin skin test