What is Glaucoma (Eye Pressure)?
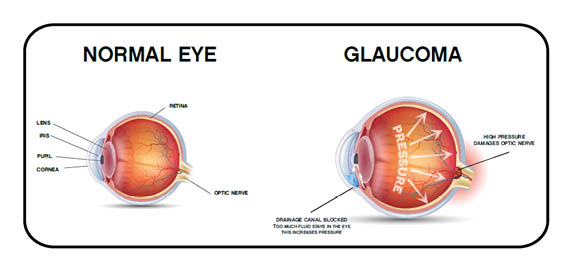
Glaucoma, popularly known as eye pressure, causes damage to the optic nerve and causes permanent vision loss. It is an insidious disease and progresses slowly. When the intraocular pressure rises, the optic nerve cells that carry signals from the retina of the eye to the brain are damaged.
This destruction caused by glaucoma is one of the most important causes of preventable vision loss. In untreated eyes, cell death, which carries signals to the brain, increases as time passes, cells cannot perform their vision function and cannot carry information to our brain.
Invisible areas do not cause complaints as they affect peripheral vision in the early period. Patients do not realize the loss of vision until the vision is affected in the center, and therefore they apply to the ophthalmologist only in the late period.
What are The Causes of Glaucoma (Eye Pressure)?
A fluid is constantly produced in the eye to nourish the intraocular tissues, and this intraocular fluid also leaves the eye continuously through some small channels. Glaucoma occurs as a result of insufficient drainage of the fluid due to the formation of structural obstruction in the channels that discharge the intraocular fluid, and the resulting increase in intraocular pressure.
Rising intraocular pressure damages the optic nerve and causes the nerve to die. In some patients, although the intraocular pressure is normal, the optic nerve is destroyed in the same way due to impaired blood flow in the optic nerve. Eye blood pressure is not related to life habits, eating and drinking, as it is to arm pressure. However, some conditions with a higher risk of glaucoma are known.
What are The Symptoms of Glaucoma (Eye Pressure)?
Glaucoma is mostly asymptomatic, and is diagnosed as a result of careful evaluation during regular eye examination. For this reason, it is also important to measure eye pressure in routine eye controls.
The main symptoms of glaucoma are:
- Decreased Vision
- Decreased Sensation of Light
- Narrowing in The Visual Field
- Eye pain
- Headache
- Bleeding in the Eye
- Nausea
- Vomiting
Who Gets Glaucoma (Eye Pressure) Most?
Although there is no definite cause of eye pressure, people with high eye pressure are in the first risk group.
However, eye pressure can be seen in anyone, even people with normal eye pressure.
-
Age:
People over the age of 40 are much more likely to have increased intraocular pressure. Having your eye pressure measured regularly after the age of 40 is very important for early diagnosis.
-
Hereditary:
If there are individuals with high intraocular pressure in other people in your family, it is more likely to occur in you.
-
Diseases Triggering Glaucoma:
High blood pressure, diabetes, heart diseases, migraine and blood circulation disorders increase the risk of intraocular pressure.
-
Eye Disorders:
The development of eye pressure is more common in patients with myopia, hyperopia, and astigmatism.
-
Eye Injuries:
As a result of a heavy blow to the eye as a result of an accident, the fluid flow in the eye can be adversely affected and accelerate the development of eye pressure.
-
Drug Uses:
Long-term use of cortisone or oral steroids can trigger eye pressure.
How Much Should Glaucoma (Eye Pressure) Be?
The eye pressure should normally be below 21 mmHg. However, this is not a definite limit. A person’s corneal thickness affects eye pressure measurements. The thicker a person’s cornea, the higher the eye pressure measurements will be.
The opposite is also true. Therefore, the thickness of the cornea of the person should be evaluated together with the measurement of eye pressure. A person with a corneal thickness of 480 and a person with a corneal thickness of 620 microns have an eye pressure of 22 mmHg, which is quite different from each other.
After eliminating the effect of corneal thickness, we can give a more correct answer to the question ‘What should the eye pressure be?’ as it is normal to be below 21 mmHg. However, sometimes glaucoma can occur even if the eye pressure is below 21 mmHg. This is called normotensive glaucoma, that is, normal pressure glaucoma.
What are The Types of Glaucoma (Eye Pressure)?
-
Open Angle Glaucoma:
It is the most common type of glaucoma and is more common after the age of 40. When the intraocular pressure rises slowly, there is no pain until the last moment, and when the disease is noticed, irreversible damage is encountered. The cause of this disease is the occurrence of resistance and obstruction in the excretory channels, which we call the trabecular meshwork, for which we do not know the exact cause. For this reason, since the eye water produced in the eye cannot be expelled, it expands the eyeball like a balloon and causes narrowing in the canal where the optic nerve passes. This stenosis also compresses the optic nerve, causing it to become compressed and dry.
-
Normotensive Glaucoma:
In this case, which we call low tension glaucoma, although the eye pressure is normal, the vessels feeding the optic nerve are damaged due to circulatory disorders.
In these patients, the eye pressure does not exceed 21 mmHg. Apart from the ophthalmic pressure of these patients, some systemic factors are also important.
They should be investigated especially in terms of anemia (Anemia), Low Blood Pressure at Night (Nocturnal Hypotension), Vasospasm (Migraine, Cold Hands or Reynaud’s Disease), Dark Blood (Hyperviscosity syndromes) and Heart Diseases.
Even the feeling of cold hands while shaking hands with these patients helps the doctor in diagnosis. In normotensive glaucoma, bleeding at the optic nerve head is more common and progresses more slowly than in Primary Open Angle Glaucoma. The first aim in the treatment of these patients is to reduce the eye pressure by 30% with drops.
-
Ocular Hypertension:
Here, although the eye pressure is high, there is no damage to the optic nerve. However, these patients should be followed very closely because of the risk of developing glaucoma in the future.
-
Angle-Closed Glaucoma:
It may be hereditary. It is more common in hypermetropes and women. In these people, the front camera is shallower and the angle of the excretory ducts is narrow.
Due to aging and especially long-term darkness, pupil dilation suddenly closes the angle and causes a glaucoma crisis. In this case, the eye pressure rises to 50-80mmHg.
In chronic angle-closure, eye pressure is above 21mmHg, vision may be normal and pain does not accompany the picture.
-
Neovascular Glaucoma:
In conditions such as diabetes (Diabetic Retinopathy) and vascular occlusion, which cause hypoxia (deprivation of oxygen) more in the retina layer, new vessels form in the iris and these new vessels increase the blood pressure by closing the angle in the anterior camera. It is a severe type of glaucoma and its treatment is difficult and takes time. Early diagnosis is very important in the treatment of this disease. Especially if ischemia is detected, ARGON LASER and Ocular Anti-VGEF treatment is very beneficial.
-
Pigmentary Glaucoma:
It is more common in 30-50 years old and myopic men. The angle is open. In these people, the iris is close to the lens and during physical activity, the pigments that give the eye color in the iris are poured into the eye water, making it difficult to outflow. Thus, the eye pressure rises. In these patients, the anterior camera is wide and the eye pressure rises up to 50mmHg. The KRUKENBERG SHUTTLE formed by iris pigments in the corneal endothelium is very typical and therefore the corneas of these patients are thicker. They may resist treatment. It should be followed carefully.
-
Exfoliative Glaucoma:
It is called pseudoexfoliative glaucoma. It is seen in older ages and the materials accumulated on the lens block the excretory channels with the movement of the iris. This type of glaucoma is associated with cataract and is resistant to treatment. It usually occurs after the age of 60. Intraocular pressure fluctuates with body position.
Since the cornea is thick in these patients, care should be taken in blood pressure measurement. In the treatment of these patients, medical therapy, especially prostaglandin analogues (drop therapy), is very useful.
In addition, LASER TRABECULOPLASTY also provides 80% success. Cataract surgery in these patients is very difficult, and therefore it must be performed with the method we call FAKO.
A round exfoliative material is seen in the middle above the lens, and this is sometimes only seen when the eye is augmented with medication. The optic nerve appearance of the same patient also shows that the disease progresses severely and rapidly.
-
Congenital Glaucoma:
In this type of blood pressure, which is present as soon as the child is born, enlargement and excessive watering occur in the eye within 1-2 months. If it is not intervened in a short time, it will result in blindness.
-
Steroid Induced Glaucoma:
Steroid (cortisone) induced glaucoma can be seen in any steroid treatment. Cortisone eye drops, cortisone pills, inhaled steroids used by asthma patients, cortisone lotions and creams applied to the face and eyelids, and cortisone injections made around or inside the eye cause glaucoma. Steroids cause an increase in eye pressure by creating resistance in the channels where eye water is discharged.
Steroid-induced glaucoma is more common in younger patients, those with diabetes, and those with high myopia. There is sensitivity to steroids at a rate of 30-40% in the society, and care should be taken in this regard.
When glaucoma develops, cortisone treatment should be stopped immediately and eye pressure should be lowered with anti-glaucoma drops if necessary. If necessary, the blood pressure should be lowered with a laser rarely.
How is Glaucoma Diagnosed?
Diagnosis of glaucoma is made through extensive and various tests. First, the patient’s glaucoma is measured with a tonometry device. Fundus examination is then performed to determine if there is any damage to the optic nerves.
After this point, if deemed necessary by the physician, multiple tests for glaucoma can be applied. In acute glaucoma crises, the diagnosis is much easier as the patient shows much more obvious symptoms. In such cases, the patient is treated urgently.
Because the later the intervention, the greater the loss of the patient’s visual field.
The methods and tests used in the diagnosis of the disease are:
- Measuring Intraocular Pressure and Examining the Drainage Angle,
- Optic Nerve Examination (Ophthalomoscopy),
- Computerized Visual Field Test,
- OCT,
- HRT,
A diagnosis of glaucoma can be achieved by applying some or all of the tests such as glaucoma.
How is Glaucoma (Eye Pressure) Treated?
-
Medication
Drops that reduce intraocular pressure are used in drug treatment. Drug treatment is preferred in cases of glaucoma detected at an early stage. The use of the drops without neglect as directed by the doctor is effective in the success of the treatment. If the intraocular pressure is regulated normally with the drop treatment, if there is no damage to the optic nerve, the treatment is continued for life without interruption. Eye pressure should be checked regularly.
-
Laser Treatment:
It is used in patients who cannot use drug therapy or who cannot tolerate drops due to side effects. Due to the development of laser technology in recent years, laser treatment methods have been successfully applied in the treatment of glaucoma.
-
Laser Iridotomy:
This laser treatment, which is extremely useful and useful in glaucoma treatment practice, is used especially in angle closure and acute glaucoma crisis, preventing possible blindness.
It should be applied as soon as the diagnosis is made. It is completed in 1-2 minutes using argon or YAG laser. The aim is to lower the blood pressure by opening a hole in the iris tissue through which the eye water will pass.
-
Laser Iridoplasty:
It is applied using an argon laser. And this is used in glaucoma crisis. It causes shrinkage of the iris. And so the front camera angle opens. It is also used in Plato Iris syndrome.
And with this method, especially in treatment-resistant neovascular glaucoma, harmful veins in the anterior camera are also burned and treated.
-
ALT (Argon Laser Trabeculoplasty):
It has been applied for years and is done with drops. The clogged channels are opened with the laser applied to the excretory channels. It is generally applied in open-angle glaucoma cases and usually after the age of 40-60. It is ineffective under the age of 25. The effect is fully visible after 3 months. It should never be applied in any situation where the angle cannot be seen.
-
SLT (Selective Laser Trabeculoplasty):
In this treatment, which is performed using a special laser, no damage is done to the excretory channels and can be safely applied many times. It is more effective than ALT and its most important feature is that it does not harm the applied area. There is no pain during this procedure and the procedure takes 1-2 minutes. Provides 20-30% blood pressure reduction. It is a safe alternative to surgical treatment, especially in patients who cannot use medication or whose blood pressure cannot be lowered despite medication.
-
Laser Cyclophotocoagulation:
This laser method is used in treatment-resistant cases. It is done by using YAG laser or DIOD laser and numbing the eye. The aim of the treatment is to reduce eye water production and lower blood pressure by affecting the ciliary body (where eye water is produced).
-
Transpupillary Cyclophotocoagulation:
This method is applied in patients who have had cataract surgery or who do not have a lens. In these patients, the ciliary body that produces eye water is directly seen and the procedure is performed with the help of a special lens using an argon laser.
-
Endoscopic Cyclophotocoagulation:
The aim here is to reduce the production of eye water, but this process is done by entering the eye with a special probe. The success rate is low in young people, and there is a 10% chance of the eye being completely extinguished (phthisis bulbi).
-
Surgical Treatment:
Purpose of surgical treatment; It is to protect the visual nerve by reducing the blood pressure, which cannot be controlled with drops or laser treatments, by surgical methods.
The most commonly used method in glaucoma surgery is the method we call trabeculectomy. Here, the liquid that accumulates in the front camera and cannot be thrown out, is created by opening another way, and it is tried to reduce the blood pressure. Glaucoma surgery has many complications and side effects. With the developing medical and laser treatments, the need for surgery is gradually decreasing.
What Should Glaucoma (Eye Pressure) Patients Pay Attention to?
- Your drops should be taken at the same time every day and as determined by your eye doctor.
- If the eye bleeding, burning etc. are observed after the use of the drug, the drug should not be discontinued, but the doctor should be consulted.
- If you are using two or more drops, take a break of at least 5 minutes between drops.
- Be sure to go to the control examinations determined by your eye doctor.
- You should also be treated to relieve other ailments such as high blood pressure, diabetes or asthma. In addition, you should pay attention to issues that are important for a healthy life, such as not smoking, regular walking and exercise.
- Medicines related to other diseases that you use or will use may affect your intraocular pressure. For this reason, you should definitely talk to your eye doctor before taking other medications.
- When you go to a doctor other than an ophthalmologist, be sure to state that you are being treated for eye pressure and the medications you are using.
- Try to notice reductions in your visual field, many patients do not realize they have this disease until they experience 40% loss of vision.
- Measuring your intraocular pressure alone is not enough for diagnosis, make sure to have the detailed analyzes we mentioned above done.